Cancer Center
BLOOD CANCER
Disease name: Blood Cancer
Blood cancer is a type of cancer that affects your blood cells. Blood cancer is caused by changes (mutations) in the DNA within blood cells. This causes the blood cells to start behaving abnormally. In almost all cases, these changes are linked to things we can’t control. Several types of cancer can form in the blood cells. Leukaemia, Lymphoma and Myeloma are some of the most common types of blood cancer. There are also types called Myelodysplastic Syndromes (MDS) and Myeloproliferative Neoplasms (MPN), are much less common.
Your treatment options will depend on several factors, such as the type and stage of your cancer, your general health, and your preferences. Together you and your doctor can weigh the benefits and risks of each cancer treatment to determine which is best for you. Treatment options for blood cancer may include:
- Chemotherapy. Chemotherapy is the major form of treatment for leukemia. This drug treatment uses chemicals to kill leukemia cells.
Depending on the type of leukemia you have, you may receive a single drug or a combination of drugs. These drugs may come in a pill form, or they may be injected directly into a vein.
- Targeted therapy. Targeted drug treatments focus on specific abnormalities present within cancer cells. By blocking these abnormalities, targeted drug treatments can cause cancer cells to die. Your leukemia cells will be tested to see if targeted therapy may be helpful for you.
- Radiation therapy. Radiation therapy uses X-rays or other high-energy beams to damage leukemia cells and stop their growth. During radiation therapy, you lie on a table while a large machine moves around you, directing the radiation to precise points on your body.
You may receive radiation in one specific area of your body where there is a collection of leukemia cells, or you may receive radiation over your whole body. Radiation therapy may be used to prepare for a bone marrow transplant.
- Bone marrow transplant. A bone marrow transplant, also called a stem cell transplant, helps reestablish healthy stem cells by replacing unhealthy bone marrow with leukemia-free stem cells that will regenerate healthy bone marrow.
Prior to a bone marrow transplant, you receive very high doses of chemotherapy or radiation therapy to destroy your leukemia-producing bone marrow. Then you receive an infusion of blood-forming stem cells that help rebuild your bone marrow.
You may receive stem cells from a donor or you may be able to use your own stem cells.
- Immunotherapy. Immunotherapy uses your immune system to fight cancer. Your body’s disease-fighting immune system may not attack your cancer because the cancer cells produce proteins that help them hide from the immune system cells. Immunotherapy works by interfering with that process.
- Engineering immune cells to fight leukemia. A specialized treatment called chimeric antigen receptor (CAR)-T cell therapy takes your body’s germ-fighting T cells, engineers them to fight cancer and infuses them back into your body. CAR-T cell therapy might be an option for certain types of leukemia.
- Clinical trials. Clinical trials are experiments to test new cancer treatments and new ways of using existing treatments. While clinical trials give you or your child a chance to try the latest cancer treatment, treatment benefits and risks may be uncertain. Discuss the benefits and risks of clinical trials with your doctor.
Tests and Procedures used to diagnose blood cancer include:
- Blood tests
- Bone marrow tests
- Imaging tests — includes CT scan, PET scan, and X-ray
- Physical exam
- Surgical lymph node removal (to use in staging)
- Physical exam. Your doctor will look for physical signs of leukemia, such as pale skin from anemia, swelling of your lymph nodes, and enlargement of your liver and spleen
- Blood tests. By looking at a sample of your blood, your doctor can determine if you have abnormal levels of red or white blood cells or platelets — which may suggest leukemia. A blood test may also show the presence of leukemia cells, though not all types of leukemia cause the leukemia cells to circulate in the blood. Sometimes the leukemia cells stay in the bone marrow
- Bone marrow test. Your doctor may recommend a procedure to remove a sample of bone marrow from your hipbone. The bone marrow is removed using a long, thin needle. The sample is sent to a laboratory to look for leukemia cells. Specialized tests of your leukemia cells may reveal certain characteristics that are used to determine your treatment options
There are several types of blood cancers, including leukemia, lymphoma, and multiple myeloma, and the medications used to treat these cancers vary depending on the type and stage of the disease. Some common medications used to treat blood cancers include:
Chemotherapy: Chemotherapy drugs are often used to treat blood cancers, and they work by killing fast-growing cancer cells. Chemotherapy can be given orally or intravenously. Some of the medications include Cytarabine (also known as Ara-C), Daunorubicin, Doxorubicin
These drugs are typically given in cycles, with treatment sessions followed by a period of rest to allow the body to recover before the next session.
Targeted therapy: Targeted therapy drugs work by targeting specific proteins or other molecules that are involved in the growth and spread of cancer cells. Examples of targeted therapy drugs include imatinib, dasatinib, and rituximab.
Immunotherapy: Immunotherapy drugs work by stimulating the patient’s immune system to recognize and attack cancer cells. Examples of immunotherapy drugs include pembrolizumab, nivolumab, and ipilimumab.
Stem cell transplant: Stem cell transplants are used to replace diseased or damaged bone marrow with healthy stem cells. The transplanted stem cells can come from the patient’s own body or from a donor.
- Cyclophosphamide: This medication is often used as part of the conditioning regimen for stem cell transplants. It is given before the transplant to help suppress the immune system and make room for the new stem cells.
- Methotrexate: Methotrexate is another medication that may be used as part of the conditioning regimen for stem cell transplants. It is given after the transplant to help prevent the new stem cells from being rejected by the patient’s immune system.
- Tacrolimus and sirolimus: These medications are immunosuppressive drugs that may be used after a stem cell transplant to help prevent the patient’s immune system from attacking the new stem cells.
- G-CSF: Granulocyte colony-stimulating factor (G-CSF) is a medication that may be used to help stimulate the production of white blood cells after a stem cell transplant.
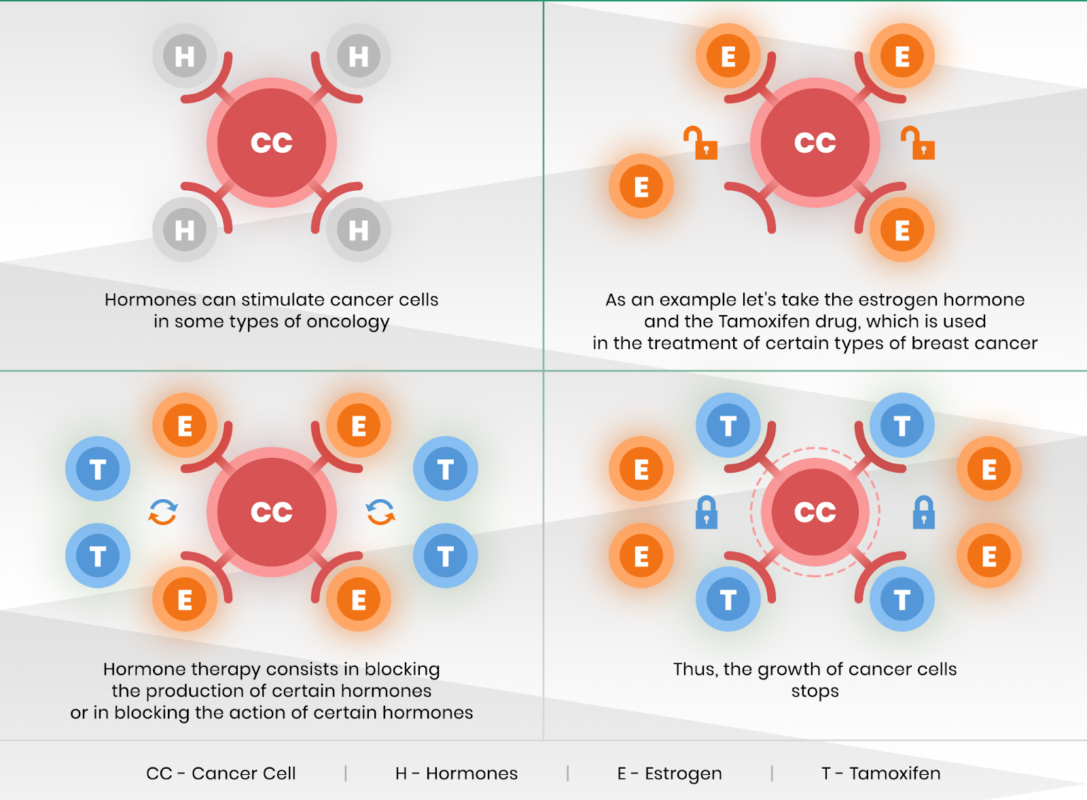
Hormone therapy: Hormone therapy drugs are used to treat some types of blood cancers that are hormone-sensitive, such as some types of leukemia.
Note:
It is important to note that the effectiveness of these drugs can vary depending on the individual and the specific type and stage of their blood cancer. It is also important to follow the guidance of a medical professional when taking any medication for blood cancer, as they can advise on potential side effects and interactions with other medications.
Procedure for Chemotherapy:

- Evaluation: Before starting chemotherapy, the patient must undergo a comprehensive medical evaluation to determine if they are a suitable candidate for the treatment. This evaluation includes blood tests, imaging studies, and consultations with an oncologist, who will determine the appropriate chemotherapy drugs and dosage based on the type and stage of cancer.
- Drug administration: Chemotherapy drugs can be administered in different ways, depending on the type of cancer being treated and the drugs used. The drugs may be given intravenously (through a vein), orally (by mouth), or topically (applied to the skin). The drugs may be given in cycles, with a period of treatment followed by a period of rest to allow the body to recover.
- Side effects management: Chemotherapy drugs can cause side effects, such as nausea, vomiting, hair loss, and fatigue. The healthcare team will monitor the patient closely for side effects and may prescribe medications or recommend other treatments to manage them.
- Follow-up care: After completing a course of chemotherapy, the patient will require ongoing follow-up care with the oncologist to monitor the cancer and assess the effectiveness of the treatment. This may involve additional imaging studies, blood tests, or other diagnostic tests.
Procedure for Immunotherapy:
Immunotherapy is a type of cancer treatment that uses the body’s immune system to recognize and destroy cancer cells. In blood cancer, there are several types of immunotherapy that can be used, including monoclonal antibodies, checkpoint inhibitors, and adoptive cell transfer.

The exact procedure for immunotherapy in blood cancer will depend on the specific type of immunotherapy being used. However, in general, the following steps may be involved:
- Diagnosis: Blood cancer is diagnosed through a variety of tests, including blood tests, bone marrow biopsies, and imaging tests.
- Consultation: Once a diagnosis is confirmed, the patient will meet with their oncologist to discuss treatment options, including immunotherapy.
- Pre-treatment evaluation: Before starting immunotherapy, the patient will undergo a series of tests to determine their overall health, including blood tests, imaging scans, and other tests as needed.
- Treatment plan: Based on the patient’s health status, the oncologist will develop a treatment plan that outlines the type of immunotherapy being used, the dosage, and the frequency of treatment.
- Administration: Immunotherapy can be given in a variety of ways, including intravenous infusion, injection, or oral medication. The method of administration will depend on the specific type of immunotherapy being used.
- Monitoring: After immunotherapy is administered, the patient will be closely monitored for side effects and to ensure the treatment is effective.
- Follow-up care: After completing the course of immunotherapy, the patient will continue to be monitored for any signs of cancer recurrence or other health issues.
Note:
It is important to note that immunotherapy can have significant side effects, and each patient’s response to treatment can vary. Patients undergoing immunotherapy should be closely monitored by their healthcare team and report any symptoms or side effects promptly.
Procedure for Radiation Therapy:
The type of radiotherapy depends on the type of cancer and the general health of the patient. The two types of radiotherapy to cure blood cancers are external and internal radiotherapy.

External beam radiotherapy procedure:
- This procedure uses a machine that aims streams of energy to the blood cancer cell through the skin.
- Radiotherapy needs constant surveillance. Before the process, the patient undergoes simulation, which measures the correct angle at which the radiation beams have to be aimed. These measurements also help in determining the proper dose of radiation.
- The procedure involves giving radiation using Linacs or linear accelerators.
- It moves around the person with a whirring noise. The radiation beam aims externally through these accelerators. The patient comes in contact with the machine.
- Only those areas with cancer cells are open to radiation, the remaining part of the body, especially the sensitive parts like ovaries and testes are under a shield.
- Therefore, scattering of radiation reduces, and the chance of skin reactions in the patients also reduces.
Internal radiation therapy procedure:
- In this therapy, the required source of radiation is inside the body. This source can be a liquid or a solid. When the liquid is used, internal radiotherapy is called systemic therapy.
- In this treatment, the source travels throughout the patient’s blood. It works by detecting the cancer cells and killing them.
- During radiation therapy, the patient’s blood count needs close supervision.
- In some cases, he/she might require blood cell transfusion. The treatment works by damaging the DNA in the cancer blood cells.
- The target of radiotherapy is to destroy the chromosomes in the DNA using extremely high radiation.
- As a result, the cells may weaken, and eventually reduces the division of the blood cancer cells. Exposure to such high emissions can immediately lead to the killing of blood cancer cells. It leads to a restriction in blood cancer cell growth. The treatment should generally cause no pain.
- Radiation therapy goes on in sessions for several weeks. The sessions will take around 30 minutes to 1 hour each, with five days a week for 7-10 weeks.
- Generally, the patient needs a break of 2-3 days for every five days to help the restoration of healthy cells.
Dosage of radiation:
Depending upon the stage of cancer, radiologists decide the dosage of treatment. The dosage depends upon the tolerance level of the patient to the procedure, too (as well). The area of treatment by radiation and the dosage mainly depends on the type of blood cancer, and its symptoms.
Side effects of radiotherapy:
Depending on the type of radiation, the area under treatment, the tolerance levels and treatment plan, radiotherapy can have healthy to adverse side effects on the patient.
The following are the most observed side effects:
- Skin problems
- Fatigue
- The decrease in blood cell count
- Variation in blood pressure and heartbeat
- Hair loss
- Dizziness
- The reduction in blood cell count
Precautions during radiotherapy:
- During the treatment, the patient has to consume enough calories and proteins as the body takes time to heal from radiation therapy.
- The patient has to take much rest. Exposure to high radiation can cause severe weakness, making them unfit for work.
- Skincare is essential too as the skin contacts radiation directly, and this can lead to damage.
- Oral health is vital. Radiation can lead to tooth decay, especially when the neck and the head are under radiation.
LUNG CANCER
Disease name: Lung Cancer
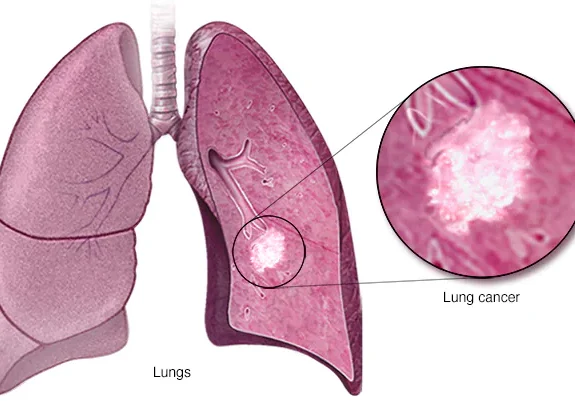
Lung cancer is a type of cancer that begins in the lungs and can spread to other parts of the body. It is the leading cause of cancer deaths worldwide, with smoking being the primary cause of the disease. There are two main types of lung cancer: non-small cell lung cancer (NSCLC) and small cell lung cancer (SCLC). NSCLC is the most common type, accounting for around 85% of all cases, while SCLC is less common but tends to grow and spread more quickly.
Symptoms of lung cancer can include a persistent cough, chest pain, shortness of breath, hoarseness, weight loss, and fatigue. Treatment options for lung cancer may include surgery, radiation therapy, chemotherapy, targeted therapy, immunotherapy, or a combination of these approaches.
There are several treatment options available for lung cancer, which may be used alone or in combination depending on the type and stage of the cancer, as well as the patient’s overall health and other factors. Here are some examples of treatments for lung cancer:
Surgery: Surgery is a common treatment for lung cancer, especially for early-stage NSCLC. The goal of surgery is to remove the tumor and any affected lymph nodes. This may involve removing a portion of the lung (lobectomy) or the entire lung (pneumonectomy).
Radiation therapy: Radiation therapy uses high-energy radiation to kill cancer cells. It may be used alone or in combination with other treatments. It can be delivered externally (external beam radiation therapy) or internally (brachytherapy).
Chemotherapy: Chemotherapy drugs can be used to kill cancer cells and stop their growth. They are typically given intravenously and may be used alone or in combination with other treatments.
Targeted therapy: Targeted therapy drugs work by targeting specific proteins or other molecules that are involved in the growth and spread of cancer cells. They may be used alone or in combination with other treatments.
Immunotherapy: Immunotherapy drugs work by stimulating the patient’s immune system to recognize and attack cancer cells. They may be used alone or in combination with other treatments.
The specific treatments used may vary depending on the type and stage of the lung cancer, as well as the patient’s overall health and other factors. It is important to follow the guidance of a medical professional when undergoing treatment for lung cancer, as they can advise on potential side effects and interactions with other medications.
Tests and procedures used to diagnose lung cancer include:
Imaging tests: Imaging tests such as X-rays, CT scans, and PET scans can help detect abnormalities in the lungs that may be indicative of cancer.
Sputum cytology: This test involves analyzing a sample of phlegm coughed up from the lungs under a microscope to look for cancer cells.
Biopsy: A biopsy involves removing a small sample of tissue from the lungs for examination under a microscope to look for cancer cells. This may be done through a needle biopsy, bronchoscopy, or surgical biopsy.
Molecular testing: Molecular testing involves analyzing a tissue sample for specific genetic mutations that may be present in lung cancer cells. This can help determine the best treatment approach for the patient.
Blood tests: Blood tests may be used to check for certain substances that may be elevated in people with lung cancer, such as tumor markers.
Lung function tests: Lung function tests may be used to assess the function of the lungs and how well they are working. This can help determine the best treatment approach for the patient.
There are several medication drugs used in the treatment of lung cancer. These may include:
Chemotherapy drugs: Chemotherapy drugs such as cisplatin, carboplatin, paclitaxel, docetaxel, and gemcitabine can be used to kill cancer cells and stop their growth. They are typically given intravenously and may be used alone or in combination with other treatments.
Targeted therapy drugs: Targeted therapy drugs such as afatinib, erlotinib, and crizotinib work by targeting specific proteins or other molecules that are involved in the growth and spread of cancer cells. They may be used alone or in combination with other treatments.
Immunotherapy drugs: Immunotherapy drugs such as pembrolizumab, nivolumab, and atezolizumab work by stimulating the patient’s immune system to recognize and attack cancer cells. They may be used alone or in combination with other treatments.
Angiogenesis inhibitors: Angiogenesis inhibitors such as bevacizumab can be used to block the growth of blood vessels that supply nutrients to cancer cells. This can help slow or stop the growth of the tumor.
Steroids: Steroids such as dexamethasone can be used to reduce inflammation and swelling in the lungs caused by lung cancer.
Note: The specific medication drugs used to treat lung cancer may vary depending on the type and stage of the cancer, as well as the patient’s overall health and other factors. It is important to follow the guidance of a medical professional when undergoing treatment for lung cancer, as they can advise on potential side effects and interactions with other medications.
Procedure for Radiation Therapy:

- Simulation: Before the actual radiation treatment, a simulation session is scheduled. During this session, the patient undergoes a CT scan to create a detailed map of the lungs and surrounding tissues. This map helps to determine the precise location and angle of the radiation beams.
- Treatment planning: The radiation oncologist and medical physicist use the information from the simulation session to create a customized treatment plan for the patient. This plan outlines the total radiation dose, the number of treatment sessions, and the exact positioning of the radiation beams.
- Radiation treatment sessions: During the actual radiation treatment sessions, the patient lies on a treatment table while a machine called a linear accelerator delivers the radiation beams to the targeted area of the lungs. The patient is positioned in the same way as during the simulation session to ensure accuracy.
- Side effects management: Radiation therapy can cause side effects such as fatigue, skin irritation, and cough. The radiation oncologist and other members of the medical team will work with the patient to manage these side effects and ensure the treatment is as comfortable as possible.
- Follow-up: After the radiation therapy is complete, the patient will have follow-up appointments with their medical team to monitor their progress and assess any potential long-term effects of the treatment.
Note:
The specific procedure for radiation therapy for lung cancer may vary depending on the individual patient and the type and stage of the cancer. It is important to consult with a medical professional if you are considering radiation therapy for lung cancer, as they can provide more detailed information on what to expect during the procedure.
Procedure for Chemotherapy:

- Treatment plan: Before beginning chemotherapy, the patient will meet with a medical oncologist who specializes in the treatment of cancer. The oncologist will review the patient’s medical history and test results and develop a customized treatment plan. This plan outlines the specific drugs, dosage, and number of treatment sessions.
- Administration: Chemotherapy drugs are typically administered through an IV (intravenously) into a vein in the patient’s arm or hand. The infusion usually takes several hours, depending on the specific drugs and dosage.
- Treatment cycles: Chemotherapy is typically given in cycles, which involve a period of treatment followed by a period of rest. The number of cycles and duration of treatment depend on the patient’s condition and the specific drugs being used.
- Side effects management: Chemotherapy can cause side effects such as nausea, fatigue, hair loss, and increased risk of infection. The oncologist and other members of the medical team will work with the patient to manage these side effects and ensure the treatment is as comfortable as possible.
- Follow-up: After chemotherapy treatment is complete, the patient will have follow-up appointments with their medical team to monitor their progress and assess any potential long-term effects of the treatment.
Note:
The specific procedure for chemotherapy for lung cancer may vary depending on the individual patient and the type and stage of the cancer. It is important to consult with a medical professional if you are considering chemotherapy for lung cancer, as they can provide more detailed information on what to expect during the procedure.
Procedure for Surgery:
Surgery is one of the treatment options for lung cancer, particularly for early-stage tumors that have not spread to other parts of the body. The specific procedure for surgery in lung cancer will depend on the size and location of the tumor, as well as the patient’s overall health status. Here are the general steps involved in the surgical procedure for lung cancer:

- Preoperative evaluation: Before surgery, the patient will undergo a series of tests to assess their overall health and determine the stage and location of the cancer. These tests may include imaging tests, blood tests, and pulmonary function tests.
- Anesthesia: The patient will be given anesthesia to ensure that they are comfortable and asleep during the surgery.
- Incision: The surgeon will make an incision in the chest wall to access the lung.
- Removal of tumor: The surgeon will remove the tumor and a small margin of healthy tissue surrounding it. This is called a lobectomy, and it involves removing the entire lobe of the lung where the tumor is located. In some cases, a smaller amount of lung tissue may be removed, known as a wedge resection or segmentectomy.
- Lymph node dissection: The surgeon may also remove nearby lymph nodes to check for the presence of cancer cells.
- Closure: After the tumor and lymph nodes have been removed, the surgeon will close the incision using sutures or staples.
- Recovery: After surgery, the patient will be closely monitored in the hospital for several days. They may have a chest tube to drain fluid from the surgical site, and will receive pain medication and other supportive care.
- Follow-up care: After leaving the hospital, the patient will continue to receive follow-up care to monitor their recovery and check for any signs of cancer recurrence.
Note:
It’s important to note that surgery can be a major procedure, and carries risks like bleeding, infection, and damage to surrounding tissues or organs. Patients undergoing lung cancer surgery should discuss the risks and benefits of the procedure with their healthcare team.
BONE CANCER
Disease Name: Bone Cancer
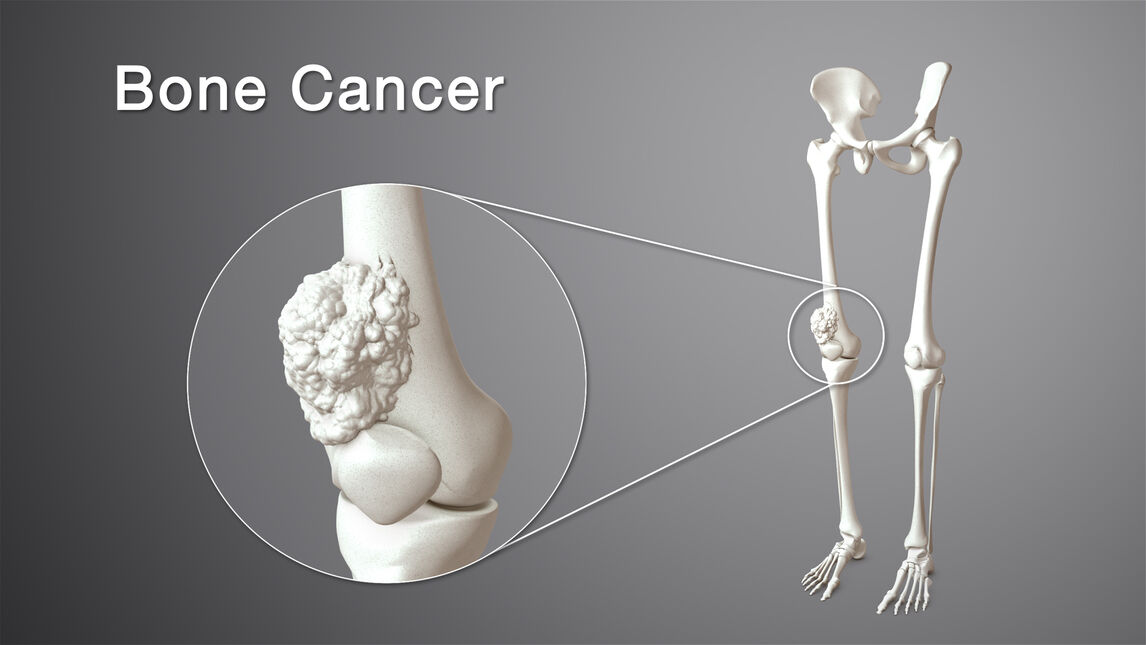
Bone cancer refers to a type of cancer that originates in the bone tissue. There are different types of bone cancer, including osteosarcoma, chondrosarcoma, and Ewing’s sarcoma, among others. Bone cancer can develop in any bone in the body, but it most commonly affects the long bones of the arms and legs, as well as the pelvis and spine. Bone cancer can be primary, meaning it originates in the bone tissue, or secondary, meaning it spreads to the bone from another part of the body. Symptoms of bone cancer may include pain, swelling, and fractures in the affected bone, as well as fatigue, weight loss, and fever.
Treatment for bone cancer depends on the type and stage of the cancer, as well as the patient’s overall health. Treatment options may include surgery, radiation therapy, chemotherapy, and targeted therapy. With early detection and appropriate treatment, many people with bone cancer are able to recover and lead fulfilling lives.
The treatment for bone cancer depends on the type and stage of the cancer, as well as the patient’s overall health. The most common treatments for bone cancer include:
- Surgery: Surgery is often the primary treatment for bone cancer. It involves removing the cancerous tumor from the bone. In some cases, the entire affected bone may need to be removed and replaced with a prosthesis or bone graft.
- Radiation therapy: Radiation therapy uses high-energy radiation to kill cancer cells. It may be used before or after surgery, or as a primary treatment for bone cancer that cannot be removed surgically. Radiation therapy may also be used to alleviate pain and other symptoms caused by bone cancer.
- Chemotherapy: Chemotherapy is a treatment that uses drugs to kill cancer cells throughout the body. It may be used in combination with surgery and/or radiation therapy for bone cancer that has spread or is at high risk of spreading.
- Targeted therapy: Targeted therapy is a treatment that uses drugs to target specific molecules or proteins involved in the growth and spread of cancer cells. It may be used in combination with other treatments for bone cancer, particularly for certain types of bone cancer that are known to have specific genetic mutations.
- Immunotherapy: Immunotherapy is a type of cancer treatment that uses the body’s immune system to fight cancer cells. It may be used in certain cases of bone cancer, particularly for those that are difficult to treat with other types of therapy.
Note:
The specific treatment for bone cancer will depend on the individual patient and the type and stage of the cancer. It is important to consult with a medical professional who specializes in the treatment of bone cancer to determine the best course of treatment for your specific situation.
Tests and procedures used to diagnose bone cancer include:
- Physical exam: A doctor will perform a physical exam to check for signs of bone cancer, such as pain or swelling in the affected area.
- Imaging tests: Imaging tests such as X-rays, CT scans, MRI scans, or bone scans can help detect abnormal areas in the bone, and determine the size and location of the tumor.
- Biopsy: A biopsy involves removing a sample of the tumor tissue for examination under a microscope. This can help determine the type of bone cancer and guide treatment decisions.
- Blood tests: Blood tests can detect certain proteins or other substances that may indicate the presence of bone cancer.
- Bone marrow biopsy: In some cases, bone cancer may spread to the bone marrow. A bone marrow biopsy involves removing a small sample of bone marrow for examination under a microscope.
- PET scan: A PET scan can be used to determine the extent of the cancer by imaging the whole body and identifying areas where the cancer has spread.
The treatment of bone cancer typically involves a combination of surgery, radiation therapy, chemotherapy, targeted therapy, and immunotherapy. Medications may be used to help manage pain, reduce inflammation, and alleviate other symptoms associated with bone cancer. Here are some of the medications commonly used in the treatment of bone cancer:
- Pain relievers: Pain relievers such as acetaminophen, nonsteroidal anti-inflammatory drugs (NSAIDs), and opioids may be used to help manage pain associated with bone cancer.
- Corticosteroids: Corticosteroids such as prednisone or dexamethasone may be used to reduce inflammation and swelling associated with bone cancer, as well as to help manage pain.
- Bisphosphonates: Bisphosphonates are drugs that help reduce bone loss and may be used to prevent or manage bone complications associated with bone cancer, such as fractures.
- Chemotherapy drugs: Chemotherapy drugs such as doxorubicin, cisplatin, and methotrexate may be used to help shrink or slow the growth of bone cancer.
- Targeted therapy drugs: Targeted therapy drugs such as denosumab and sunitinib may be used to target specific molecules or proteins involved in the growth and spread of bone cancer cells.
- Immunotherapy drugs: Immunotherapy drugs such as checkpoint inhibitors may be used to stimulate the immune system to attack cancer cells.
Note:
The specific medications used to treat bone cancer will depend on the individual patient and the type and stage of the cancer. It is important to consult with a medical professional who specializes in the treatment of bone cancer to determine the best course of treatment for your specific situation.
Procedure for Surgery:

- Pre-surgery preparation: Prior to surgery, your medical team will perform a thorough evaluation to determine the extent and stage of the cancer. This may involve imaging tests, such as X-rays, MRI, CT scans, or bone scans.
- Anesthesia: You will be given general anesthesia to ensure that you are comfortable and asleep during the procedure.
- Incision: The surgeon will make an incision in the skin over the affected bone to access the tumor.
- Removal of tumor: The surgeon will carefully remove the tumor, as well as a margin of healthy tissue around it to ensure that all of the cancer cells have been removed.
- Reconstruction: Depending on the extent of the surgery, reconstruction may be necessary to restore function to the affected bone. This may involve using bone grafts or other materials to rebuild the bone.
- Closure: Once the tumor has been removed and any necessary reconstruction has been performed, the incision will be closed using sutures or staples.
- Recovery: After the surgery, you will be monitored in the hospital for a period of time to ensure that you are recovering properly. You may need to use crutches, a brace, or other devices to support the affected bone while it heals.
Note:
The specific details of the surgical procedure will depend on the individual patient and the type and stage of the cancer. It is important to consult with a medical professional who specializes in the treatment of bone cancer to determine the best course of treatment for your specific situation.
Procedure for Radiation Therapy:

- Pre-treatment planning: Before beginning radiation therapy, your medical team will perform a thorough evaluation to determine the extent and stage of the cancer, as well as the size and location of the tumor. This may involve imaging tests, such as X-rays, MRI, CT scans, or bone scans.
- Marking the treatment area: To ensure that the radiation is targeted precisely to the tumor, the treatment area will be marked on the skin using small tattoos or markers.
- Radiation therapy sessions: You will receive radiation therapy in a series of sessions, which may last several weeks. During each session, you will lie on a table and a machine will deliver the radiation to the targeted area.
- Monitoring: Throughout the course of treatment, your medical team will monitor your progress and adjust the radiation dosage as needed.
- Follow-up care: After the course of radiation therapy is complete, you will be monitored closely to ensure that the cancer has been effectively treated. You may also need additional treatment, such as surgery or chemotherapy, depending on the extent and stage of the cancer.
Note:
The specific details of the radiation therapy procedure will depend on the individual patient and the type and stage of the cancer. It is important to consult with a medical professional who specializes in the treatment of bone cancer to determine the best course of treatment for your specific situation.
Procedure for Chemotherapy:

- Pre-treatment evaluation: Before beginning chemotherapy, your medical team will perform a thorough evaluation to determine the extent and stage of the cancer, as well as your overall health. This may involve blood tests, imaging tests, such as X-rays, MRI, CT scans, or bone scans, and other diagnostic tests.
- Administering chemotherapy drugs: Chemotherapy drugs can be given in different ways, depending on the type and stage of the cancer. They may be given orally as a pill, intravenously (through an IV), or through a catheter or port that is placed directly into a vein.
- Monitoring: During chemotherapy, your medical team will closely monitor your response to the drugs and adjust the dosage as needed.
- Managing side effects: Chemotherapy can cause a range of side effects, such as nausea, vomiting, fatigue, and hair loss. Your medical team will work to manage these side effects to help you feel as comfortable as possible during treatment.
- Follow-up care: After the course of chemotherapy is complete, you will be monitored closely to ensure that the cancer has been effectively treated. You may also need additional treatment, such as surgery or radiation therapy, depending on the extent and stage of the cancer.
Note:
The specific details of the chemotherapy procedure will depend on the individual patient and the type and stage of the cancer. It is important to consult with a medical professional who specializes in the treatment of bone cancer to determine the best course of treatment for your specific situation.
BRAIN CANCER
Disease name: Brain Cancer

Brain cancer refers to the growth of abnormal cells in the brain or the tissues surrounding the brain. These abnormal cells can form a tumor that can interfere with the normal functioning of the brain and nervous system. Brain tumors can be either benign (non-cancerous) or malignant (cancerous), and can arise from different types of cells in the brain. The symptoms of brain cancer can vary depending on the location, size, and type of tumor. Common symptoms include headaches, seizures, nausea or vomiting, changes in vision or hearing, weakness or numbness in the limbs, difficulty speaking or understanding language, and changes in mood or behavior. However, these symptoms can also be caused by other conditions, so it’s important to see a healthcare provider if you experience any of these symptoms.
There are different treatment options available for brain cancer, including surgery, radiation therapy, and chemotherapy. The specific treatment approach depends on the type and location of the tumor, as well as the patient’s overall health and other factors. Brain cancer can be a serious condition, but early detection and prompt treatment can help improve outcomes for patients.
The treatment for brain cancer depends on various factors such as the type and location of the tumor, its size and growth rate, as well as the patient’s age and overall health. Here are the most common treatment options for brain cancer:
- Surgery: Surgical removal of the tumor is often the first-line treatment for brain cancer. A surgeon will attempt to remove as much of the tumor as possible without causing damage to the surrounding brain tissue. In some cases, the entire tumor may not be able to be removed.
- Radiation therapy: Radiation therapy uses high-energy radiation beams to kill cancer cells. It may be used before or after surgery or as a primary treatment for tumors that cannot be removed surgically. There are different types of radiation therapy, including external beam radiation therapy and brachytherapy.
- Chemotherapy: Chemotherapy uses drugs to kill cancer cells. It can be given orally or intravenously and may be used in combination with radiation therapy. Chemotherapy drugs can also be delivered directly to the brain through a thin tube inserted through the skull.
- Targeted therapy: Targeted therapy uses drugs that target specific proteins or genes that are present in cancer cells, but not in healthy cells. This type of therapy may be used in combination with other treatments, such as chemotherapy and radiation therapy.
- Immunotherapy: Immunotherapy is a newer treatment option that uses the body’s own immune system to fight cancer cells. It works by stimulating the immune system to recognize and attack cancer cells. Immunotherapy may be used alone or in combination with other treatments.
Note:
The specific treatment plan for brain cancer will depend on various factors, and treatment may involve a combination of different approaches. A healthcare provider who specializes in the treatment of brain cancer can help determine the best treatment plan for each individual patient.
Tests and procedures used to diagnose brain cancer include:
- Neurological exam: This is a physical exam that assesses the patient’s neurological function, including their reflexes, muscle strength, coordination, and sensation.
- Imaging tests: Imaging tests such as magnetic resonance imaging (MRI) or computed tomography (CT) scans can create detailed images of the brain to detect abnormalities such as tumors.
- Biopsy: A biopsy is a procedure in which a sample of tissue is removed from the brain and examined under a microscope to determine if it is cancerous or non-cancerous.
- Blood tests: Blood tests can be used to detect certain tumor markers or to evaluate the patient’s overall health.
- Lumbar puncture: A lumbar puncture (also known as a spinal tap) is a procedure in which a small amount of cerebrospinal fluid (CSF) is removed from the spinal canal and analyzed for signs of cancer.
There are several types of medication drugs that may be used to treat brain cancer, depending on the type and stage of the cancer. Here are some of the most common medication drugs used for brain cancer treatment:
- Chemotherapy: Chemotherapy drugs are used to kill cancer cells by stopping them from dividing and growing. Common chemotherapy drugs used for brain cancer include temozolomide, carmustine, and lomustine.
- Targeted therapy: Targeted therapy drugs are designed to attack specific proteins or other molecules that are present in cancer cells, while leaving normal cells unharmed. For brain cancer, targeted therapy drugs such as bevacizumab and cetuximab may be used.
- Immunotherapy: Immunotherapy drugs work by stimulating the immune system to recognize and attack cancer cells. Immune checkpoint inhibitors such as nivolumab and pembrolizumab are sometimes used for certain types of brain cancer.
- Hormone therapy: Hormone therapy drugs may be used for brain tumors that are hormone-sensitive, meaning that they grow in response to certain hormones in the body. Hormone therapy drugs such as tamoxifen and aromatase inhibitors may be used in some cases.
- Anti-epileptic drugs: Anti-epileptic drugs are sometimes used to treat seizures that may occur as a result of brain cancer.
Note:
The choice of medication drugs for brain cancer treatment will depend on the individual patient’s circumstances, including the type and stage of the cancer, as well as the patient’s overall health and other factors. A healthcare provider who specializes in the treatment of brain cancer can help determine the appropriate medication regimen for each patient.
Procedure for Chemotherapy:

The procedure for chemotherapy for brain cancer involves several steps:
- Planning: Before chemotherapy treatment begins, the healthcare provider will perform tests to determine the extent of the cancer and the most appropriate chemotherapy drugs to use. They will also discuss the possible side effects of chemotherapy and the steps to take to manage them.
- Administration: Chemotherapy drugs can be given in several ways, including orally, intravenously (IV), or directly into the cerebrospinal fluid (CSF) through a catheter placed in the brain. The method of administration will depend on the type and location of the cancer, as well as the patient’s overall health.
- Treatment schedule: The frequency and duration of chemotherapy treatment will depend on the type and stage of the cancer, as well as the chemotherapy drugs used. Typically, chemotherapy treatment is given in cycles, with a period of rest between cycles to allow the body to recover.
- Monitoring: During chemotherapy treatment, the patient will be closely monitored for any side effects or complications. Blood tests may be done to check the patient’s blood cell counts and liver function.
- Adjustments: Depending on the patient’s response to chemotherapy and any side effects experienced, adjustments may be made to the dosage or schedule of chemotherapy drugs.
Note:
It’s important for patients to communicate any symptoms or side effects they experience during chemotherapy treatment to their healthcare provider, who can provide guidance and support to manage them.
Procedure for Hormone Therapy:
Hormone therapy is typically not used as a first-line treatment for brain cancer. However, in some cases, hormone therapy may be used in combination with other treatments to slow the growth of certain types of brain tumors, such as meningiomas or pituitary adenomas.
The specific procedure for hormone therapy in brain cancer will depend on the type of hormone therapy being used. Here are the general steps involved in the procedure:
- Diagnosis: Brain cancer is diagnosed through a variety of tests, including imaging scans, biopsies, and blood tests.
- Consultation: Once a diagnosis is confirmed, the patient will meet with their oncologist to discuss treatment options, including hormone therapy.
- Hormone evaluation: Before starting hormone therapy, the patient will undergo a series of tests to determine the type of hormone receptors present in their tumor.
- Treatment plan: Based on the patient’s health status and the type of hormone receptors present in their tumor, the oncologist will develop a treatment plan that outlines the type of hormone therapy being used, the dosage, and the frequency of treatment.
- Hormone therapy administration: Hormone therapy can be given in a variety of ways, including oral medication or injection. The method of administration will depend on the specific type of hormone therapy being used.
- Monitoring: After hormone therapy is administered, the patient will be closely monitored for side effects and to ensure the treatment is effective.
- Follow-up care: After completing the course of hormone therapy, the patient will continue to be monitored for any signs of cancer recurrence or other health issues.
Note:
It is important to note that hormone therapy can have significant side effects, and each patient’s response to treatment can vary. Patients undergoing hormone therapy should be closely monitored by their healthcare team and report any symptoms or side effects promptly.
Procedure for Immunotherapy:
Immunotherapy is a type of cancer treatment that harnesses the body’s immune system to attack and destroy cancer cells. The procedure for immunotherapy for brain cancer may involve the following steps:

- Diagnosis: The first step in immunotherapy for brain cancer is usually a diagnosis. This may involve imaging tests such as MRI or CT scans, as well as a biopsy to determine the type and grade of the brain tumor.
- Evaluation of immune system: The healthcare team may evaluate the patient’s immune system to determine whether it is strong enough to undergo immunotherapy. This may involve blood tests and other evaluations.
- Selection of immunotherapy treatment: Based on the type and stage of brain cancer, as well as the patient’s overall health, the healthcare team can determine the appropriate type of immunotherapy treatment. Some examples of immunotherapy treatments include immune checkpoint inhibitors, CAR T-cell therapy, and tumor-infiltrating lymphocyte therapy.
- Treatment administration: Immunotherapy for brain cancer may be administered intravenously through an infusion or injection, or through a specific delivery method such as a wafer placed into the brain during surgery. The duration and frequency of treatment may vary depending on the specific immunotherapy treatment.
- Monitoring and follow-up: Throughout the course of immunotherapy, the healthcare team will monitor the patient’s response to treatment using imaging tests and other measures. The patient may also be monitored for potential side effects or complications of the treatment. Based on the patient’s response to treatment, the healthcare team may adjust the treatment plan as needed.
Note:
It is important to note that immunotherapy for brain cancer is still a developing field, and the success of treatment can vary depending on the specific type and stage of the cancer, as well as the patient’s overall health. Immunotherapy may also be used in combination with other treatments for brain cancer, such as surgery, radiation therapy, and chemotherapy.
LIVER CANCER
Disease name: Liver Cancer
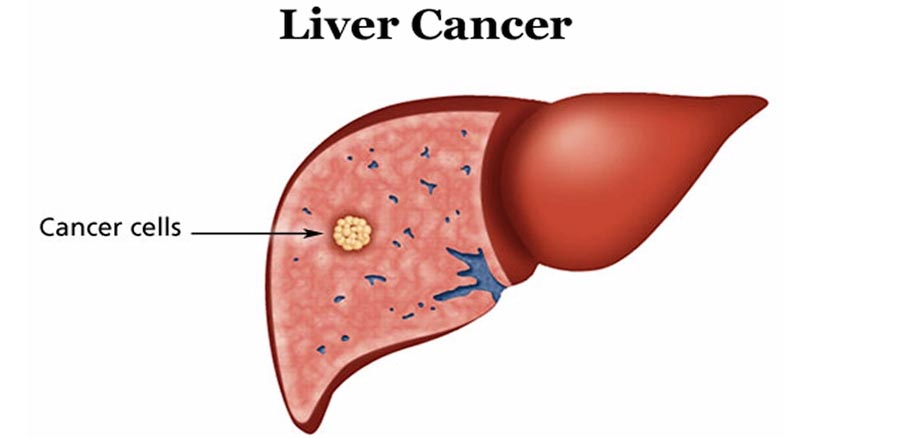
Liver cancer is cancer that begins in the cells of your liver. Your liver is a football-sized organ that sits in the upper right portion of your abdomen, beneath your diaphragm and above your stomach. Several types of cancer can form in the liver. The most common type of liver cancer is hepatocellular carcinoma, which begins in the main type of liver cell (hepatocyte). Other types of liver cancer, such as intrahepatic cholangiocarcinoma and hepatoblastoma, are much less common.
The treatment for liver cancer depends on several factors, including the type and stage of the cancer, as well as the patient’s overall health. Treatment options for liver cancer may include:
- Surgery: If the cancer is confined to the liver, surgery to remove the tumor or the affected portion of the liver may be an option.
- Liver transplant: In some cases, a liver transplant may be recommended, particularly if the cancer is limited to the liver and the patient has cirrhosis or other liver damage.
- Radiation therapy: Radiation therapy uses high-energy radiation to kill cancer cells. It may be used alone or in combination with other treatments.
- Chemotherapy: Chemotherapy uses drugs to kill cancer cells. It may be given orally or through a vein.
- Immunotherapy: Immunotherapy uses drugs to stimulate the immune system to recognize and attack cancer cells.
- Targeted therapy: Targeted therapy uses drugs to specifically target and block the growth and spread of cancer cells.
In some cases, a combination of treatments may be used. It’s important to talk with your doctor about the best treatment options for you based on your individual situation.
Tests and procedures used to diagnose liver cancer include:
- Blood tests. Blood tests may reveal liver function abnormalities.
- Imaging tests. Your doctor may recommend imaging tests, such as an ultrasound, CT and MRI.
- Removing a sample of liver tissue for testing. Sometimes it’s necessary to remove a piece of liver tissue for laboratory testing in order to make a definitive diagnosis of liver cancer.
During a liver biopsy, your doctor inserts a thin needle through your skin and into your liver to obtain a tissue sample. In the lab, doctors examine the tissue under a microscope to look for cancer cells. Liver biopsy carries a risk of bleeding, bruising and infection.
There are several types of medications that can be used to treat liver cancer, depending on the stage of the cancer, the patient’s overall health, and other factors. Some of the common medications used to treat liver cancer include:
- Chemotherapy drugs: These drugs are used to kill cancer cells by stopping their ability to divide and grow. Common chemotherapy drugs used to treat liver cancer include cisplatin, doxorubicin, and fluorouracil.
- Targeted therapy drugs: These drugs are designed to specifically target certain proteins or genes that are involved in the growth and spread of cancer cells. Some examples of targeted therapy drugs used to treat liver cancer include sorafenib and Lenvatinib.
- Immunotherapy drugs: These drugs help to stimulate the patient’s immune system to recognize and attack cancer cells. Checkpoint inhibitors, such as nivolumab and pembrolizumab, are examples of immunotherapy drugs used to treat liver cancer.
- Hormone therapy drugs: These drugs are used to block the hormones that stimulate the growth of certain types of liver cancer. For example, hormonal therapy may be used to treat hepatocellular carcinoma (HCC) that has spread outside the liver and cannot be treated with surgery or ablation.
- Radiopharmaceuticals: These are radioactive drugs that can be given either intravenously or orally, which will then travel to the liver and emit radiation, killing cancer cells.
Note:
It’s important to note that the choice of medication(s) for liver cancer treatment depends on the specific type, stage, and characteristics of the cancer, as well as the patient’s overall health and other medical conditions. It’s crucial to talk with a medical professional about the best treatment options for each individual case.
Procedure for liver transplant:
Liver transplantation is a surgical procedure in which a diseased or damaged liver is replaced with a healthy liver from a donor. Here are the general steps involved in the liver transplant process:
- Evaluation: Before a liver transplant, the patient must undergo a comprehensive medical evaluation to determine if they are a suitable candidate for the surgery. This evaluation includes blood tests, imaging studies, and consultations with a transplant team, which typically includes a surgeon, hepatologist, and other healthcare professionals.
- Waitlisting: If the patient is deemed a suitable candidate for a liver transplant, they will be placed on a waitlist for a donor liver. The wait time can vary, depending on the patient’s condition, blood type, and the availability of donor livers.
- Surgery: Once a suitable donor liver becomes available, the transplant surgery will be performed. The surgery typically takes several hours and is performed under general anesthesia. The surgeon will remove the patient’s diseased liver and replace it with the healthy donor liver. The blood vessels and bile ducts in the new liver will be connected to the patient’s blood vessels and bile ducts.
- Recovery: After the surgery, the patient will be closely monitored in the hospital for several days to ensure that the new liver is functioning properly. The recovery time can vary, but most patients can expect to spend several weeks in the hospital.
- Follow-up care: After being discharged from the hospital, the patient will require ongoing follow-up care with the transplant team. This includes regular check-ups, blood tests, and imaging studies to monitor the function of the new liver and ensure that the patient is not experiencing any complications.
Note:
It’s important to note that the liver transplant process can vary depending on the individual patient’s case and the specific transplant center where the surgery is performed. If you are considering a liver transplant, it’s important to consult with a qualified healthcare professional who can provide more information about the procedure and answer any questions you may have.
Procedure for Chemotherapy:
Chemotherapy is a treatment for cancer that involves the use of drugs to kill cancer cells. The procedure for chemotherapy can vary depending on the type and stage of cancer, the drugs used, and the patient’s overall health. Here are the general steps involved in the chemotherapy process:

- Evaluation: Before starting chemotherapy, the patient must undergo a comprehensive medical evaluation to determine if they are a suitable candidate for the treatment. This evaluation includes blood tests, imaging studies, and consultations with an oncologist, who will determine the appropriate chemotherapy drugs and dosage based on the type and stage of cancer.
- Drug administration: Chemotherapy drugs can be administered in different ways, depending on the type of cancer being treated and the drugs used. The drugs may be given intravenously (through a vein), orally (by mouth), or topically (applied to the skin). The drugs may be given in cycles, with a period of treatment followed by a period of rest to allow the body to recover.
- Side effects management: Chemotherapy drugs can cause side effects, such as nausea, vomiting, hair loss, and fatigue. The healthcare team will monitor the patient closely for side effects and may prescribe medications or recommend other treatments to manage them.
- Follow-up care: After completing a course of chemotherapy, the patient will require ongoing follow-up care with the oncologist to monitor the cancer and assess the effectiveness of the treatment. This may involve additional imaging studies, blood tests, or other diagnostic tests.
Note:
It’s important to note that the chemotherapy process can vary depending on the individual patient’s case and the specific cancer being treated. If you are considering chemotherapy, it’s important to consult with a qualified healthcare professional who can provide more information about the procedure and answer any questions you may have.
Procedure for Immunotherapy:
Immunotherapy is a type of cancer treatment that involves using the body’s immune system to fight cancer. The procedure for immunotherapy can vary depending on the type of immunotherapy being used and the specific cancer being treated. Here are the general steps involved in the immunotherapy process:

- Evaluation: Before starting immunotherapy, the patient must undergo a comprehensive medical evaluation to determine if they are a suitable candidate for the treatment. This evaluation includes blood tests, imaging studies, and consultations with an oncologist, who will determine the appropriate immunotherapy drug and dosage based on the type and stage of cancer.
- Drug administration: Immunotherapy drugs can be administered in different ways, depending on the type of cancer being treated and the drugs used. Some immunotherapy drugs are given intravenously (through a vein), while others are given orally (by mouth). The drugs may be given in cycles, with a period of treatment followed by a period of rest to allow the body to recover.
- Side effects management: Immunotherapy drugs can cause side effects, such as fatigue, fever, chills, and muscle aches. The healthcare team will monitor the patient closely for side effects and may prescribe medications or recommend other treatments to manage them.
- Follow-up care: After completing a course of immunotherapy, the patient will require ongoing follow-up care with the oncologist to monitor the cancer and assess the effectiveness of the treatment. This may involve additional imaging studies, blood tests, or other diagnostic tests.
Note:
It’s important to note that the immunotherapy process can vary depending on the individual patient’s case and the specific cancer being treated. If you are considering immunotherapy, it’s important to consult with a qualified healthcare professional who can provide more information about the procedure and answer any questions you may have.
KIDNEY CANCER
Disease Name: Kidney Cancer

Kidney cancer, also known as renal cell carcinoma, is a type of cancer that begins in the cells of the kidneys. It is one of the most common types of cancer in adults and typically affects people over the age of 40.
The exact cause of kidney cancer is not known, but there are several risk factors that may increase the likelihood of developing the disease, including:
- Smoking
- Obesity
- High blood pressure
- Long-term dialysis treatment
- Family history of kidney cancer
- Exposure to certain chemicals, such as asbestos or cadmium
Symptoms of kidney cancer may include:
- Blood in the urine
- A lump or mass in the side or lower back
- Pain in the side or lower back that does not go away
- Weight loss
- Loss of appetite
- Fatigue
Diagnosis of kidney cancer typically involves a physical exam, medical history, imaging tests (such as CT scans or MRI), and a biopsy (removal of a small piece of tissue for examination under a microscope).
Treatment for kidney cancer can vary depending on the stage and type of the cancer, but typically involves surgery to remove the tumor and surrounding tissue, as well as targeted therapy, immunotherapy, or a combination of treatments. It’s important to work closely with a team of healthcare professionals to develop the best treatment plan for your individual case.
Medications for kidney cancer:
There are several medications used to treat kidney cancer, including:
- Targeted therapies: These drugs are designed to target specific molecules or pathways involved in cancer cell growth and can be used in patients with advanced kidney cancer. Some examples include sunitinib (Sutent), pazopanib (Votrient), axitinib (Inlyta), and cabozantinib (Cabometyx).
- Immunotherapies: These drugs help the body’s immune system to recognize and attack cancer cells. The most commonly used immunotherapies for kidney cancer are checkpoint inhibitors, such as nivolumab (Opdivo) and pembrolizumab (Keytruda), which block the PD-1/PD-L1 pathway.
- Chemotherapy: Chemotherapy drugs, such as gemcitabine and cisplatin, can be used to treat advanced kidney cancer, but they are generally less effective than targeted therapies and immunotherapies.
- Hormone therapy: This type of therapy is used to treat rare types of kidney cancer, such as renal cell carcinoma with sarcomatoid features, which may be hormone-sensitive. Hormone therapy can involve drugs such as medroxyprogesterone acetate (MPA) or tamoxifen.
Note:
It’s important to note that the specific medications used to treat kidney cancer can vary depending on factors such as the stage and type of the cancer, the patient’s overall health, and other individual factors. Treatment plans are typically developed by a team of healthcare professionals, including oncologists, urologists, and other specialists, in consultation with the patient.
Kidney cancer treatments:
Treatment for kidney cancer can vary depending on several factors, including the stage and type of the cancer, the location and size of the tumor, the patient’s overall health, and other individual factors. Here are some of the most common treatment options for kidney cancer:
- Surgery: The most common treatment for kidney cancer is surgery to remove the tumor and surrounding tissue. Depending on the location and size of the tumor, the surgeon may perform a partial nephrectomy (removal of only the tumor and a portion of the kidney) or a radical nephrectomy (removal of the entire kidney). In some cases, minimally invasive laparoscopic or robotic surgery may be an option.
- Radiation therapy: Radiation therapy uses high-energy X-rays or other types of radiation to kill cancer cells. This is not a common treatment for kidney cancer but may be used in some cases.
- Targeted therapy: Targeted therapy is a type of treatment that uses drugs to target specific molecules or pathways that contribute to cancer cell growth. This is a common treatment for advanced kidney cancer and may be used in combination with other therapies.
- Immunotherapy: Immunotherapy is a type of treatment that uses drugs to help the body’s immune system recognize and attack cancer cells. This is also a common treatment for advanced kidney cancer and may be used in combination with other therapies.
- Chemotherapy: Chemotherapy drugs are used to kill cancer cells and may be used in some cases of kidney cancer, but it is generally less effective than targeted therapy and immunotherapy.
- Clinical trials: There are ongoing clinical trials testing new treatments for kidney cancer, including new targeted therapies, immunotherapies, and combination therapies.
Note:
It’s important to note that the best treatment plan for kidney cancer will depend on several factors, and treatment plans are typically developed by a team of healthcare professionals, including oncologists.
Procedure for Surgery:
Surgery is one of the treatment options for kidney cancer, particularly for early-stage tumors that have not spread to other parts of the body. The specific procedure for surgery in kidney cancer will depend on the size and location of the tumor, as well as the patient’s overall health status. Here are the general steps involved in the surgical procedure for kidney cancer:

- Preoperative evaluation: Before surgery, the patient will undergo a series of tests to assess their overall health and determine the stage and location of the cancer. These tests may include imaging tests, blood tests, and pulmonary function tests.
- Anesthesia: The patient will be given anesthesia to ensure that they are comfortable and asleep during the surgery.
- Incision: The surgeon will make an incision in the side or abdomen to access the kidney.
- Removal of tumor: The surgeon will remove the tumor and a small margin of healthy tissue surrounding it. This is called a partial nephrectomy, and it involves removing only the part of the kidney where the tumor is located. In some cases, a larger portion of the kidney may need to be removed, called a radical nephrectomy.
- Lymph node dissection: The surgeon may also remove nearby lymph nodes to check for the presence of cancer cells.
- Closure: After the tumor and lymph nodes have been removed, the surgeon will close the incision using sutures or staples.
- Recovery: After surgery, the patient will be closely monitored in the hospital for several days. They may have a urinary catheter and a drainage tube to drain fluid from the surgical site, and will receive pain medication and other supportive care.
- Follow-up care: After leaving the hospital, the patient will continue to receive follow-up care to monitor their recovery and check for any signs of cancer recurrence.
Note:
It’s important to note that surgery can be a major procedure, and carries risks like bleeding, infection, and damage to surrounding tissues or organs. Patients undergoing kidney cancer surgery should discuss the risks and benefits of the procedure with their healthcare team.
Procedure for Radiation therapy:

Radiation therapy is not typically used as a primary treatment for kidney cancer, but may be used in certain cases to help manage symptoms or to treat cancer that has spread to other parts of the body. Here are the general steps involved in the procedure for radiation therapy for kidney cancer:
- Simulation: Before radiation therapy can begin, the patient will undergo a simulation session to plan the treatment. During this session, the patient will lie on a table in the same position they will be in during treatment, and imaging tests like CT scans or MRIs will be used to create a 3D image of the tumor and surrounding tissues.
- Treatment planning: Using the 3D images created during the simulation session, the radiation oncologist will develop a treatment plan that determines the appropriate dose and area of the kidney to target with radiation.
- Radiation therapy administration: During radiation therapy, the patient will lie on a table and a machine called a linear accelerator will deliver high-energy radiation beams to the affected area of the kidney. The treatment is painless and takes only a few minutes.
- Monitoring: After each radiation therapy session, the patient will be closely monitored by their healthcare team for any side effects or complications. Depending on the treatment plan, the patient may undergo several radiation therapy sessions over a period of several weeks.
- Follow-up care: After completing radiation therapy, the patient will receive follow-up care to monitor their recovery and check for any signs of cancer recurrence. They may also receive supportive care to manage any side effects of the treatment.
Note:
It is important to note that radiation therapy can have significant side effects, including fatigue, skin irritation, and damage to surrounding tissues. Patients undergoing radiation therapy should discuss the risks and benefits of the procedure with their healthcare team.
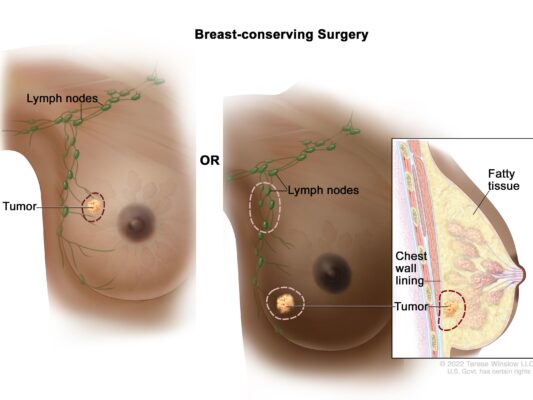
BREAST CANCER
Disease Name: Breast Cancer
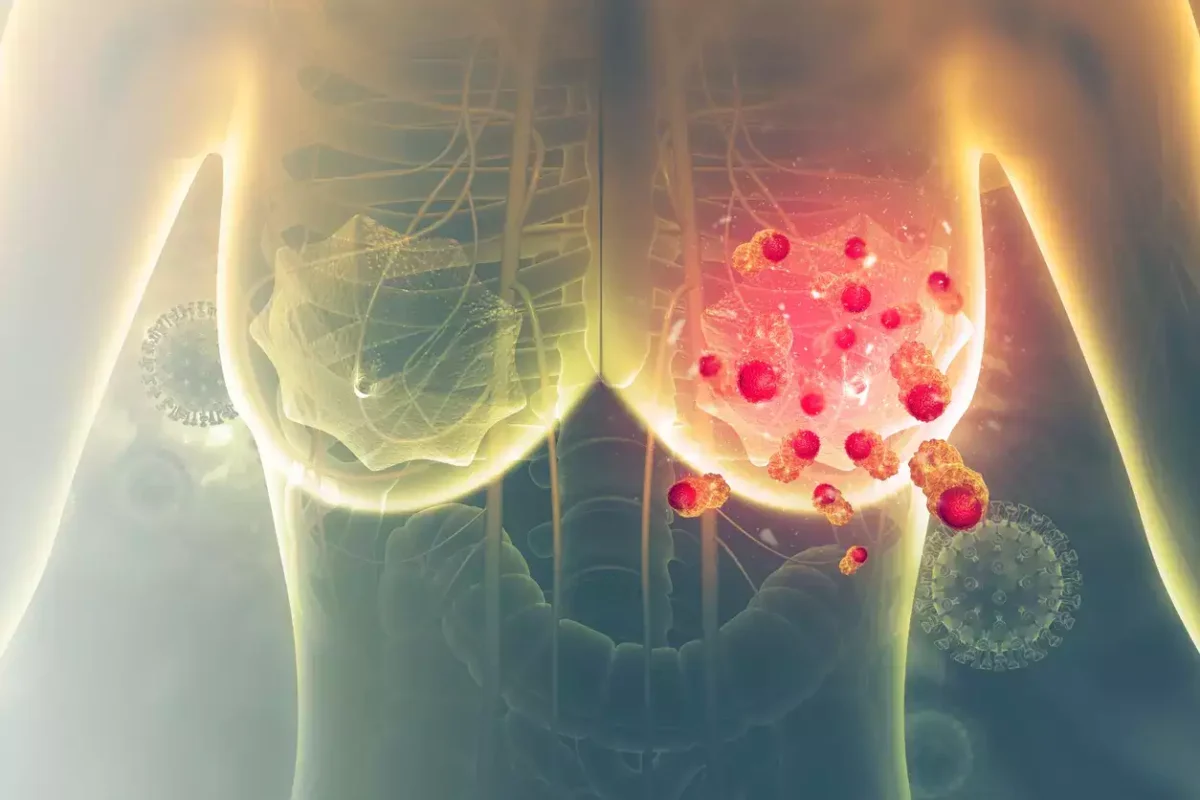
Breast cancer is a type of cancer that develops in breast tissue. It is the most common cancer among women worldwide and can also occur in men. Breast cancer occurs when cells in the breast grow abnormally and form a tumor.
These cancerous cells can spread to other parts of the body, including the lymph nodes and other organs, through the bloodstream or lymphatic system. Early detection and treatment are crucial for improving the chances of survival from breast cancer. Screening tests, such as mammograms, can detect breast cancer in its early stages when it is most treatable. Treatment options for breast cancer may include surgery, radiation therapy, chemotherapy, hormone therapy, targeted therapy, or a combination of these approaches.
Several risk factors are associated with breast cancer, including age, gender, family history, certain genetic mutations, hormonal factors, lifestyle factors such as diet and exercise, and exposure to certain environmental factors. Breast cancer can have a significant impact on a person’s physical, emotional, and social well-being. Support from healthcare providers, family, and friends is important for those affected by breast cancer.
The treatment for breast cancer depends on several factors, including the stage and type of cancer, the patient’s overall health, and their preferences.
Here are some of the common treatments for breast cancer:
- Surgery: Surgery is the most common treatment for breast cancer. It involves removing the cancerous tumor and some surrounding tissue. Types of surgery include lumpectomy, mastectomy, and lymph node removal.
- Radiation therapy: Radiation therapy uses high-energy rays to kill cancer cells. It is often used after surgery to kill any remaining cancer cells or to shrink tumors before surgery.
- Chemotherapy: Chemotherapy uses drugs to kill cancer cells. It can be given before surgery to shrink the tumor or after surgery to kill any remaining cancer cells.
- Hormone therapy: Hormone therapy is used to treat breast cancers that are hormone receptor-positive. It involves blocking the hormones that can cause breast cancer cells to grow.
- Targeted therapy: Targeted therapy is a type of treatment that targets specific proteins or genes that are involved in the growth and spread of cancer cells.
- Immunotherapy: Immunotherapy is a type of treatment that helps the body’s immune system fight cancer cells. In addition to these treatments, there are also clinical trials available that offer patients access to new and innovative treatments. Treatment plans are tailored to each patient’s unique needs, and it’s important to discuss all treatment options with a healthcare provider to make an informed decision.
Tests and procedures used to diagnose breast cancer include:
There are several tests and procedures that may be used to diagnose breast cancer. These include:
- Breast exam: A doctor will perform a physical examination of the breasts to check for any lumps, changes in texture or shape, or other abnormalities.
- Mammogram: A mammogram is an X-ray of the breast tissue that can detect abnormalities, such as lumps or calcifications, that may be cancerous.
- Breast ultrasound: A breast ultrasound uses high-frequency sound waves to create images of the breast tissue. It can help determine if a lump is solid or fluid-filled (cystic).
- Breast magnetic resonance imaging (MRI): A breast MRI uses a magnetic field and radio waves to create detailed images of the breast tissue. It is often used in combination with a mammogram for women at high risk of breast cancer.
- Biopsy: A biopsy involves removing a small amount of tissue from the breast to examine under a microscope. There are several types of biopsy, including core needle biopsy, fine needle aspiration, and surgical biopsy.
- Genetic testing: Genetic testing may be recommended for individuals with a family history of breast cancer or those who have certain risk factors. The test can determine if an individual has inherited mutations in genes such as BRCA1 or BRCA2, which increase the risk of developing breast cancer.
Note:
It’s important to note that not all abnormalities found on imaging tests or during a physical exam are cancerous, and further testing may be necessary to make a definitive diagnosis. A healthcare provider can help determine which tests are most appropriate for an individual based on their specific situation.
There are several medications used to treat breast cancer. The type of medication prescribed depends on the type and stage of the cancer, as well as the patient’s individual situation. Here are some common medications used to treat breast cancer:
- Hormone therapy: Hormone therapy is often used to treat breast cancers that are hormone receptor-positive. Medications used in hormone therapy include tamoxifen, aromatase inhibitors, and ovarian suppression drugs.
- Chemotherapy: Chemotherapy uses drugs to kill cancer cells. Common chemotherapy drugs used to treat breast cancer include anthracyclines, taxanes, and cyclophosphamide.
- Targeted therapy: Targeted therapy is a type of medication that targets specific proteins or genes that are involved in the growth and spread of cancer cells. Examples of targeted therapy drugs used to treat breast cancer include trastuzumab and lapatinib.
- Immunotherapy: Immunotherapy is a type of medication that helps the body’s immune system fight cancer cells. Pembrolizumab is a type of immunotherapy that may be used to treat certain types of breast cancer.
- Bisphosphonates: Bisphosphonates are medications used to strengthen bones and may be prescribed to patients with breast cancer that has spread to the bones.
Note:
It’s important to note that not all medications are appropriate for all patients, and the decision to prescribe a medication depends on several factors, including the patient’s overall health, the type and stage of the cancer, and the potential side effects of the medication. A healthcare provider can help determine which medications are most appropriate for an individual based on their specific situation.
Procedure for Chemotherapy:
The procedure for chemotherapy for breast cancer may vary depending on the type and stage of cancer and the individual’s health status. However, there are some general steps that are typically involved in the chemotherapy process:
- Chemotherapy drugs are administered through a vein (intravenously) using a needle or a catheter. The drugs may be given in a hospital, clinic, or doctor’s office.
- Before starting chemotherapy, the healthcare provider may check the individual’s blood counts and other lab values to ensure they are healthy enough to receive treatment.
- The chemotherapy drugs may be given in cycles, with rest periods in between. The length and number of cycles may vary depending on the specific chemotherapy regimen.
- During chemotherapy, the individual may experience side effects, such as nausea, vomiting, fatigue, and hair loss. Healthcare providers may prescribe medications to help manage these side effects.
- After completing chemotherapy, the healthcare provider may perform follow-up tests, such as imaging scans, to evaluate the effectiveness of treatment.
Note:
It’s important to note that chemotherapy may not be appropriate for all individuals with breast cancer, and the decision to undergo chemotherapy depends on several factors, including the stage and type of cancer, the individual’s overall health, and their personal preferences. A healthcare provider can help determine if chemotherapy is the right treatment option for an individual based on their specific situation.
Procedure for targeted therapy:
The procedure for targeted therapy for breast cancer may vary depending on the specific medication being used and the individual’s health status. However, there are some general steps that are typically involved in the targeted therapy process:
- The healthcare provider will order tests to determine if the individual’s breast cancer is HER2-positive or has other specific mutations that can be targeted by medication.
- If the individual is a candidate for targeted therapy, the healthcare provider will prescribe the appropriate medication, such as trastuzumab or lapatinib.
- Targeted therapy medications are typically administered intravenously or orally, depending on the specific medication being used.
- During targeted therapy, the individual may experience side effects, such as nausea, diarrhea, or heart problems, depending on the medication being used. Healthcare providers may prescribe medications to manage these side effects.
- After completing targeted therapy, the healthcare provider may perform follow-up tests, such as imaging scans or blood tests, to evaluate the effectiveness of treatment.
BLADDER CANCER
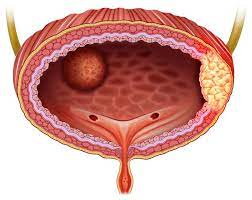
Disease Name: Bladder Cancer

Bladder cancer is a type of cancer that occurs in the tissues of the bladder, which is a hollow organ located in the pelvis that stores urine until it is expelled from the body. Bladder cancer usually begins in the cells lining the inside of the bladder and can spread to other parts of the body if left untreated. It is the sixth most common type of cancer in the United States, with men being three to four times more likely to develop bladder cancer than women.
Common risk factors for bladder cancer include smoking, exposure to certain chemicals, chronic bladder inflammation, and a family history of bladder cancer. Symptoms of bladder cancer may include blood in the urine, frequent urination, pain or burning during urination, and lower back pain. Treatment for bladder cancer depends on the stage and location of the cancer and may include surgery, chemotherapy, radiation therapy, and immunotherapy. Early detection and treatment of bladder cancer can greatly improve the chances of a positive outcome, so it’s important to see a healthcare provider if any symptoms of bladder cancer are present.
The treatment for bladder cancer depends on several factors, including the stage and grade of the cancer, the individual’s overall health, and personal preferences. Here are some common treatments for bladder cancer:
- Surgery: Surgery is often the first-line treatment for bladder cancer. The type of surgery depends on the stage and location of the cancer. Transurethral resection of bladder tumor (TURBT) is a common surgical procedure used to remove early-stage bladder cancer. Radical cystectomy, which involves removing the entire bladder, may be necessary for more advanced cases.
- Chemotherapy: Chemotherapy uses drugs to kill cancer cells. Chemotherapy may be given before or after surgery or in combination with radiation therapy. The drugs may be given intravenously or directly into the bladder through a catheter.
- Radiation therapy: Radiation therapy uses high-energy radiation to kill cancer cells. Radiation therapy may be given before or after surgery or in combination with chemotherapy. The radiation may be delivered externally or internally through a catheter placed in the bladder.
- Immunotherapy: Immunotherapy is a type of medication that helps the body’s immune system fight cancer cells. Bacillus Calmette-Guerin (BCG) is a type of immunotherapy that is commonly used to treat early-stage bladder cancer.
Note:
It’s important to note that not all treatments are appropriate for all patients, and the decision to pursue a particular treatment depends on several factors, including the individual’s overall health, the stage and grade of the cancer, and potential side effects of the treatment. A healthcare provider can help determine which treatments are most appropriate for an individual based on their specific situation.
Tests and procedures used to diagnose bladder cancer include:
There are several tests and procedures that can be used to diagnose bladder cancer. Here are some of the most common:
- Urine tests: A urine sample may be collected and tested for the presence of blood, cancer cells, or other abnormal cells.
- Cystoscopy: A cystoscope is a thin, flexible tube with a camera and light on the end that is inserted through the urethra into the bladder. This allows the healthcare provider to examine the inside of the bladder and collect tissue samples for further testing.
- Imaging tests: Imaging tests, such as CT scans, MRIs, and ultrasounds, can be used to get a detailed look at the bladder and surrounding tissues.
- Biopsy: During a biopsy, a sample of tissue is removed from the bladder and examined under a microscope to look for cancer cells.
- Staging tests: If bladder cancer is diagnosed, additional tests may be performed to determine the stage of the cancer and whether it has spread to other parts of the body. These may include additional imaging tests, bone scans, or other procedures.
Note:
It’s important to note that not all of these tests may be necessary for every individual with suspected bladder cancer, and the specific tests used depend on the individual’s symptoms, medical history, and other factors. A healthcare provider can help determine which tests are most appropriate for an individual based on their specific situation.
There are several types of medication drugs that may be used to treat bladder cancer, including:
- Chemotherapy drugs: Chemotherapy drugs can be used to kill cancer cells or slow their growth. They may be given intravenously or directly into the bladder through a catheter. Common chemotherapy drugs used for bladder cancer include cisplatin, gemcitabine, and paclitaxel.
- Immunotherapy drugs: Immunotherapy drugs help the body’s immune system to recognize and attack cancer cells. The most common type of immunotherapy used for bladder cancer is Bacillus Calmette-Guerin (BCG), which is a type of bacteria that is used to stimulate the immune system to attack cancer cells.
- Targeted therapy drugs: Targeted therapy drugs are designed to target specific proteins or other molecules that are involved in the growth and spread of cancer cells. These drugs may be used in combination with other treatments, such as chemotherapy or radiation therapy. Common targeted therapy drugs used for bladder cancer include pembrolizumab, nivolumab, and atezolizumab.
- Hormone therapy drugs: Hormone therapy drugs may be used to treat advanced bladder cancer that has spread to other parts of the body. These drugs work by blocking hormones that can promote the growth of cancer cells. Hormone therapy is less commonly used for bladder cancer than for other types of cancer, such as breast or prostate cancer.
Note:
It’s important to note that not all medication drugs are appropriate for all patients, and the decision to pursue a particular medication depends on several factors, including the individual’s overall health, the stage and grade of the cancer, and potential side effects of the medication. A healthcare provider can help determine which medications are most appropriate for an individual based on their specific situation.
Procedure for Chemotherapy:
Chemotherapy for bladder cancer can be given in several different ways, depending on the individual’s specific situation. Here are some common procedures for chemotherapy for bladder cancer:
- Intravenous (IV) chemotherapy: This is the most common way chemotherapy is given for bladder cancer. Chemotherapy drugs are administered through a needle or catheter that is inserted into a vein, usually in the arm. The drugs are delivered directly into the bloodstream and circulate throughout the body, targeting cancer cells.
- Intravesical chemotherapy: This type of chemotherapy is delivered directly into the bladder through a catheter. The chemotherapy drugs are held in the bladder for a short period of time (usually an hour or less) before being drained out. This type of chemotherapy is typically used for early-stage bladder cancer that has not spread beyond the lining of the bladder.
- Combination therapy: Combination therapy involves using two or more chemotherapy drugs at the same time. This may be done through IV infusion or intravesical instillation. Combination therapy is often used for more advanced bladder cancer or cancer that has spread beyond the bladder.
- Neoadjuvant chemotherapy: Neoadjuvant chemotherapy is chemotherapy that is given before surgery to remove the bladder (radical cystectomy). The goal of neoadjuvant chemotherapy is to shrink the tumor and make it easier to remove. This type of chemotherapy is typically given through IV infusion.
- Adjuvant chemotherapy: Adjuvant chemotherapy is chemotherapy that is given after surgery to remove the bladder. The goal of adjuvant chemotherapy is to kill any remaining cancer cells and reduce the risk of the cancer coming back. Adjuvant chemotherapy is typically given through IV infusion.
Note:
During chemotherapy treatment, the individual will need to come in for regular appointments to receive the chemotherapy drugs and monitor their progress. The exact treatment schedule and duration of chemotherapy will depend on the individual’s specific situation and the type of chemotherapy being used.
Procedure for Immunotherapy:
Immunotherapy is a type of treatment for bladder cancer that works by helping the body’s immune system to recognize and attack cancer cells. Here is a general overview of the procedure for immunotherapy for bladder cancer:
- Consultation: Before starting immunotherapy, a healthcare provider will review the individual’s medical history, perform a physical exam, and run tests to determine if immunotherapy is the best course of treatment for the individual’s specific situation.
- Immunotherapy medications: The most common type of immunotherapy used for bladder cancer is Bacillus Calmette-Guerin (BCG). BCG is a type of bacteria that is used to stimulate the immune system to attack cancer cells. The BCG is given through a catheter that is inserted into the bladder. The BCG is left in the bladder for a short period of time (usually one to two hours) before being drained out.
- Treatment schedule: The exact treatment schedule for immunotherapy will depend on the individual’s specific situation. BCG immunotherapy is typically given in a series of treatments that are spaced out over several weeks or months. During this time, the individual will need to come in for regular appointments to receive the immunotherapy and monitor their progress.
- Side effects: Like all cancer treatments, immunotherapy can have side effects. The most common side effects of BCG immunotherapy include flu-like symptoms, such as fever, chills, and fatigue. It is also common for individuals to experience bladder irritation or discomfort during and after the procedure.
- Monitoring: After completing the course of immunotherapy, the individual will need to continue to come in for regular appointments to monitor their progress and check for any signs of recurrence. If the cancer comes back, additional treatments may be necessary.
Note:
It’s important to note that not all individuals with bladder cancer are candidates for immunotherapy, and the decision to pursue immunotherapy depends on several factors, including the individual’s overall health, the stage and grade of the cancer, and potential side effects of the treatment. A healthcare provider can help determine if immunotherapy is an appropriate treatment option for an individual based on their specific situation.
SINUS CANCER
Disease Name: Sinus Cancer
Sinus cancer is a rare cancer that affects the nasal cavity (the space behind your nose) and the sinuses (small air-filled cavities inside your nose, cheekbones and forehead). Nasal and sinus cancer is different from cancer of the area where the nose and throat connect. This is called nasopharyngeal cancer.
The treatment for Sinus cancer depends on several factors, including the type and stage of the cancer, as well as the patient’s overall health. Treatment options for Sinus Cancer may include:
- Chemotherapy
- Radiation Therapy
- Surgery
Chemotherapy- Chemotherapy is typically used in conjunction with radiation to treat sinus cancer. In general, chemotherapy, or a combination of chemotherapy and radiation therapy, tends to be used before surgery or after surgery as an additional treatment for sinus cancers. For patients with widespread (metastatic) sinus cancer, or those who are unable to withstand surgery, chemotherapy alone or in combination with other options may be used as the main treatment option.
Radiation therapy- Radiation therapy is often used in conjunction with surgery. Patients may undergo radiation treatment before or after the surgical procedure. Radiation may also be used in conjunction with chemotherapy. Radiation therapy may also be an option for melanoma or sarcoma of the nasal cavity or sinuses. For sphenoid sinus cancer, which occurs in the bones directly behind the nose, radiation therapy may be the primary treatment used, as surgical removal of a tumor in this area may be difficult to perform successfully and safely.
Surgery- Surgery is a central part of treatment for most sinus cancers. Combined with other treatments like chemotherapy and radiation therapy, surgery to remove the tumor often results in the most favorable outcomes for patients with sinus cancer. Surgical procedures to treat sinus cancer may involve:
Excision: Surgeons may remove tumors and some local tissue during an excision. This procedure is typically performed on early-stage cancers, for small nasal cavity tumors.
Endoscopic sinus surgery: This minimally invasive procedure may be used on early-stage nasal or sinus cancer patients. A thin tube, or endoscope, is inserted into an incision in the sinus or nasal cavity to remove tumors. It’s less invasive than other sinus cancer surgeries that require cutting and opening up the nasal cavity (open surgeries). This operation may have a quicker recovery time and, when done by experienced surgeons on eligible cancers, may be just as successful as more aggressive surgical methods.
Maxillectomy: This operation removes all or part (partial maxillectomy) of the hard palate, the front of the roof of the mouth. A special denture can be created to fill the hole formed by this surgery. Your doctor will likely refer you to a prosthodontist, a specialized dentist, who can make a prosthetic tailored to your mouth. This surgery may be used for nasal cavity cancers that grow on the nasal cavity wall or for maxillary sinus cancers. For early-stage maxillary sinus cancers (stages 0, 1 and 2), a maxillectomy is often the first treatment option used.
Microvascular reconstruction: Microvascular reconstruction surgery uses tissues from other parts of the body, such as a rib graft or ear cartilage, to rebuild the upper jaw or other areas impacted by tissue removal following a maxillectomy. Surgeons use a microscope to connect blood vessels from the free flap in the neck to keep the recently transplanted tissue alive and healthy.
Free flaps: Using microvascular surgery, in which small blood vessels are sewn together under a microscope, reconstructing the sinuses may be possible by using tissue and muscle from other areas of the body, such as the intestines, arm, leg or abdomen.
Tests and procedures used to diagnose Sinus Cancer include:
Biopsy
Biopsies are performed after CT scans and MRIs are completed. A biopsy is used to confirm the presence of cancer in the nasal cavity or paranasal sinus. A sample of tissues or cells is required for a biopsy, which must be conducted before treatment begins. Biopsies may also help to measure the aggressiveness of the cancer, and where it originated.
The types of biopsies typically used in diagnosing sinus cancers are:
Incisional biopsy: A small piece of tissue is cut from an abnormal-looking area. If the abnormal region is easily accessed, the sample may be taken at your doctor’s office. If the tumor is located deeper within the sinus, the biopsy may need to be performed in an operating room with anesthesia administered for pain. The sample may also be obtained through a more involved endoscopic or open surgical biopsy.
Excisional biopsy: The entire tumor or lesion is removed from a suspicious area. If the region is easily accessed, the sample may be taken in a physician’s office. If the tumor is deep inside the sinus, an operating room may be required, along with anesthesia for pain. A more involved endoscopic or open surgical biopsy may be necessary.
Fine needle aspiration (FNA): A very thin needle attached to a syringe is used to extract cells from a tumor or lump.
Endoscopic biopsy: Tumors and tissue in hard-to-reach places may be obtained through the use of an endoscope, or thin, lighted tube.
Open biopsy: An open surgical biopsy may be required to access tumors or tissue deep inside the sinuses. This may involve cutting skin and bones around the nose to reach the tumors.
Endoscopy
An endoscope may be inserted into the nose so that your doctor can examine hard-to-see areas such as the nasal and sinus passages, and internal and posterior parts of the nose.
Imaging tests
CT scan: The cross-sectional view provided by the CT scan may help locate abnormalities or tumors in the sinus area. We also may use the CT to measure tumor size, to determine if existing sinus cancer is growing or metastasizing into the eye or brain, and assess bony parts of the nasal cavity and paranasal sinus areas. Dye may be used to provide better contrast and image clarity.
MRI: An MRI may help study the soft tissue and identify cancers in the paranasal sinuses and nasal cavities. It also may offer insight into whether sinus cancer has spread to the eye or brain.
Procedure for Chemotherapy:
Chemotherapy is a type of cancer treatment that uses drugs to kill cancer cells. It may be used alone or in combination with other treatments for sinus cancer, depending on the stage and type of the cancer. The procedure for chemotherapy in sinus cancer typically involves the following steps:
- Evaluation and diagnosis: The first step is to undergo an evaluation to determine the type and stage of the cancer. This may involve imaging tests, such as CT or MRI scans, and a biopsy to confirm the diagnosis.
- Treatment planning: Once the cancer is diagnosed, the oncologist will develop a treatment plan that may include chemotherapy, radiation therapy, surgery, or a combination of these treatments.
- Chemotherapy administration: Chemotherapy drugs may be given orally, by injection, or through an intravenous (IV) infusion. The frequency and duration of treatment will depend on the type and stage of the cancer.
- Monitoring and management of side effects: Chemotherapy can cause a range of side effects, such as nausea, vomiting, fatigue, hair loss, and decreased blood cell counts. The oncologist will monitor the patient’s progress and manage any side effects that arise.
- Follow-up care: After completing chemotherapy, the patient will require ongoing monitoring and follow-up care to monitor for any signs of recurrence or long-term side effects.
Note:
It is important to note that the specific procedure for chemotherapy in sinus cancer may vary depending on the individual case and the treatment plan developed by the oncologist. It is also important to discuss any questions or concerns with the healthcare team to ensure a clear understanding of the treatment process and potential side effects.
Procedure for Radiation Therapy:
Radiation therapy is a common treatment for sinus cancer. It uses high-energy radiation to kill cancer cells and shrink tumors. Here is an overview of the procedure for radiation therapy in sinus cancer:
- Simulation: The first step is to determine the precise location of the tumor and the surrounding healthy tissue. This is done through a process called simulation, which involves using imaging techniques such as CT or MRI scans to create a detailed map of the area being treated.
- Treatment planning: Once the simulation is complete, the radiation oncologist will develop a treatment plan that outlines the dose and schedule of radiation. The goal is to deliver enough radiation to kill cancer cells while minimizing damage to healthy tissue.
- Radiation treatment: The actual radiation treatment involves the use of a machine called a linear accelerator. The machine delivers a high-energy beam of radiation to the tumor and surrounding tissue. The individual will lie on a treatment table and the machine will move around them to deliver radiation from different angles. Each treatment session typically lasts 15-30 minutes, and the total number of sessions will depend on the size and stage of the tumor.
- Follow-up: After radiation therapy, the individual will need to attend follow-up appointments to monitor their recovery and to ensure that the cancer does not return. Additional treatment, such as surgery or chemotherapy, may be necessary if the cancer has spread or if there is a high risk of recurrence.
Note:
It’s important to note that radiation therapy can cause side effects, such as fatigue, skin irritation, and changes in taste and smell. These side effects are usually temporary and can be managed with medication or other treatments. Your healthcare provider can provide more detailed information about the radiation therapy procedure and what to expect during recovery.
Procedure for Surgery:
Surgery is a common treatment for sinus cancer. The type of surgery will depend on the size and location of the tumor, as well as the individual’s overall health. Here is an overview of the procedure for surgery in sinus cancer:
- Anesthesia: The individual will be given general anesthesia to ensure that they are asleep and pain-free during the procedure.
- Incision: The surgeon will make an incision in the skin or inside the nose to access the tumor.
- Tumor removal: The surgeon will remove as much of the tumor as possible while preserving nearby healthy tissue. This may involve removing part or all of the affected sinus, as well as nearby bone and tissue.
- Reconstruction: Depending on the extent of the surgery, the surgeon may need to reconstruct the affected area using grafts, implants, or other materials.
- Closure: Once the tumor has been removed and the area has been reconstructed, the surgeon will close the incision with sutures or staples.
- Follow-up: After surgery, the individual will need to attend follow-up appointments to monitor their recovery and to ensure that the cancer does not return. Additional treatment, such as radiation therapy or chemotherapy, may be necessary if the cancer has spread or if there is a high risk of recurrence.
Note:
It’s important to note that surgery for sinus cancer can cause side effects, such as pain, bleeding, and infection. These side effects are usually temporary and can be managed with medication or other treatments. Your healthcare provider can provide more detailed information about the surgery procedure and what to expect during recovery.
SKIN CANCER
Disease Name: Skin Cancer

Skin cancer is the out-of-control growth of abnormal cells in the epidermis, the outermost skin layer, caused by unrepaired DNA damage that triggers mutations. These mutations lead the skin cells to multiply rapidly and form malignant tumors.
The treatment for Skin cancer depends on several factors, including the type and stage of the cancer, as well as the patient’s overall health. Treatment options for Skin Cancer may include:
- Freezing
- Excisional Surgery
- Mohs Surgery
- Radiation Therapy
- Chemotherapy
- Photodynamic Therapy
- Biological Therapy
Freezing- Your doctor may destroy actinic keratoses and some small, early skin cancers by freezing them with liquid nitrogen (cryosurgery). The dead tissue sloughs off when it thaws.
Excisional surgery- This type of treatment may be appropriate for any type of skin cancer. Your doctor cuts out (excises) the cancerous tissue and a surrounding margin of healthy skin. A wide excision removing extra normal skin around the tumor may be recommended in some cases.
Mohs surgery- This procedure is for larger, recurring or difficult-to-treat skin cancers, which may include both basal and squamous cell carcinomas. It’s often used in areas where it’s necessary to conserve as much skin as possible, such as on the nose.
Radiation therapy- Radiation therapy uses high-powered energy beams, such as X-rays, to kill cancer cells. Radiation therapy may be an option when cancer can’t be completely removed during surgery.
Chemotherapy- In chemotherapy, drugs are used to kill cancer cells. For cancers limited to the top layer of skin, creams or lotions containing anti-cancer agents may be applied directly to the skin. Systemic chemotherapy can be used to treat skin cancers that have spread to other parts of the body.
Photodynamic therapy- This treatment destroys skin cancer cells with a combination of laser light and drugs that makes cancer cells sensitive to light.
Biological therapy- Biological therapy uses your body’s immune system to kill cancer cells.
Tests and procedures used to diagnose Skin Cancer include:
Biopsy
In many cases, your doctor will remove the whole growth. During this procedure, your doctor will numb the area before removing a tissue sample.
There are several different biopsy methods, but an excisional biopsy in which the doctor removes the entire growth is often sufficient to treat the skin cancer.
Other types of biopsies include a shave biopsy, in which your doctor shaves off the top layers of the lesion, and a punch biopsy, in which the doctor uses a special tool to cut a tiny round piece of the tumor, including deeper layers of the skin.
Your doctor may also take a biopsy of any suspicious lymph nodes to see if they contain cancer cells.
Imaging tests
Most skin cancers especially basal cell carcinoma, the most common form of skin cancer remain local and do not spread to distant organs. Melanoma and Merkel cell carcinoma are more prone to spread. In those cases, one of several medical imaging procedures may be used to determine whether cancer cells have metastasized to internal organs and bones. Imaging procedures include:
- CT Scan
- X–ray
- MRI
These imaging procedures are non-invasive and painless. If they reveal suspicious spots or metastases, a more invasive biopsy may be required.
Procedure for Mohs Surgery:
Mohs surgery is a specialized surgical procedure used to treat certain types of skin cancer. The procedure is designed to remove the cancerous cells while preserving as much healthy tissue as possible. Here is an overview of the procedure for Mohs surgery in skin cancer:
- Anesthesia: Mohs surgery is typically performed under local anesthesia, which means the individual will be awake but numb in the area being treated.
- Removal of visible tumor: The surgeon will remove the visible tumor using a scalpel. The area is then bandaged and the individual will wait while the tissue sample is processed and analyzed.
- Mapping and analysis of the tissue sample: The removed tissue sample is divided into sections and mapped onto a diagram. The tissue is then processed and analyzed under a microscope to determine if any cancerous cells remain.
- Further tissue removal: If cancerous cells are found in the analyzed tissue, the surgeon will remove an additional layer of tissue from the affected area, focusing specifically on the area where cancerous cells were found.
- Repeating the analysis process: The tissue is again processed and analyzed under a microscope to determine if any cancerous cells remain. This process is repeated until no cancerous cells are found in the analyzed tissue.
- Closure: Once the surgeon is confident that all cancerous cells have been removed, the wound is closed using sutures or other methods.
- Follow-up: After Mohs surgery, the individual will need to attend follow-up appointments to monitor their recovery and to ensure that the cancer does not return.
Note:
It’s important to note that Mohs surgery can cause side effects, such as pain, swelling, and scarring. However, the procedure is designed to minimize the amount of healthy tissue that is removed, which can help to reduce the risk of complications and promote faster healing. Your healthcare provider can provide more detailed information about the Mohs surgical procedure and what to expect during recovery.
Procedure for Excisional Surgery:
Excisional surgery is a common procedure used to treat many types of skin cancer, including basal cell carcinoma, squamous cell carcinoma, and melanoma. The procedure involves removing the cancerous lesion and a surrounding margin of healthy skin to ensure that all cancer cells have been removed. Here is an overview of the procedure for excisional surgery in skin cancer:
- Anesthesia: Excisional surgery is typically performed under local anesthesia, which means the individual will be awake but numb in the area being treated.
- Removal of the lesion: The surgeon will use a scalpel to remove the cancerous lesion along with a surrounding margin of healthy skin. The size of the margin will depend on the size and location of the lesion, as well as other factors such as the type and stage of the cancer.
- Closure: Once the lesion has been removed, the wound is closed using sutures or other methods. The size and shape of the wound will depend on the size and location of the lesion, as well as the size of the margin of healthy tissue that was removed.
- Pathology evaluation: The tissue that was removed is sent to a laboratory for evaluation under a microscope to determine if all of the cancer cells have been removed. This evaluation may take several days.
- Follow-up: After excisional surgery, the individual will need to attend follow-up appointments to monitor their recovery and to ensure that the cancer does not return. Additional treatment, such as radiation therapy or chemotherapy, may be necessary if the cancer has spread or if there is a high risk of recurrence.
Note:
It’s important to note that excisional surgery can cause side effects, such as pain, swelling, and scarring. However, the procedure is designed to remove all of the cancer cells while preserving as much healthy tissue as possible. Your healthcare provider can provide more detailed information about the excisional surgical procedure and what to expect during recovery.
Procedure for Photodynamic therapy:
Photodynamic therapy (PDT) is a treatment option for some types of skin cancer, including basal cell carcinoma and squamous cell carcinoma. The procedure involves using a special solution, called a photosensitizing agent, and a specific wavelength of light to destroy cancerous cells. Here is an overview of the procedure for photodynamic therapy in skin cancer:
- Application of photosensitizing agent: A photosensitizing agent, such as aminolevulinic acid (ALA) or methyl aminolevulinate (MAL), is applied to the skin in the area being treated. The agent is absorbed by the cancerous cells and makes them more sensitive to light.
- Incubation period: The photosensitizing agent is left on the skin for a period of time, typically 1-3 hours. During this time, the agent is absorbed by the cancerous cells and healthy cells are unaffected.
- Light therapy: After the incubation period, a specific wavelength of light is applied to the area being treated. The light activates the photosensitizing agent, which destroys the cancerous cells while sparing healthy tissue. The light source can be a laser or other type of light-emitting device.
- Follow-up: After photodynamic therapy, the individual will need to attend follow-up appointments to monitor their recovery and to ensure that the cancer does not return. Additional treatment, such as excisional surgery or radiation therapy, may be necessary if the cancer has spread or if there is a high risk of recurrence.
Note:
It’s important to note that photodynamic therapy can cause side effects, such as redness, swelling, and peeling of the skin in the treated area. These side effects are usually temporary and resolve within a few weeks. Your healthcare provider can provide more detailed information about the photodynamic therapy procedure and what to expect during recovery.
THYROID CANCER
Disease Name: Thyroid Cancer
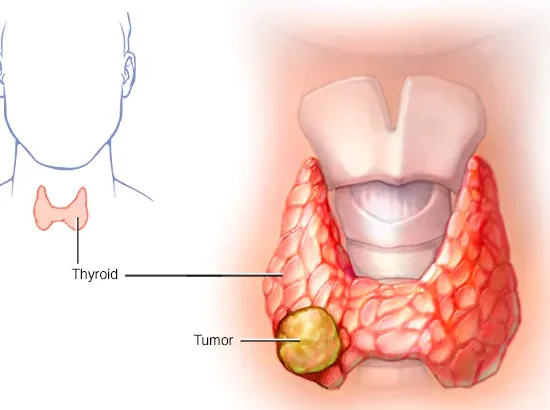
Thyroid cancer is a type of cancer that starts in the thyroid gland. Cancer starts when cells begin to grow out of control. Thyroid cancer develops in your thyroid gland, a part of your endocrine system. Your thyroid gland produces hormones that regulate body temperature, heart rate and metabolism. Most thyroid cancers are highly curable.
The treatment for Thyroid cancer depends on several factors, including the type and stage of the cancer, as well as the patient’s overall health. Treatment options for Thyroid Cancer may include:
- Surgery
- Radioactive Iodine (Radioiodine) Therapy
- Thyroid Hormone Therapy
- External Beam Radiation Therapy
- Chemotherapy
Surgery– Thyroidectomy is surgery to remove the thyroid gland. It is the most common surgery for thyroid cancer. As with lobectomy, this is typically done through an incision a few inches long across the front of the neck.
Radioactive Iodine (Radioiodine) Therapy– It is rarely used to treat thyroid cancer, but it’s sometimes used to treat anplastic thyroid carcinomas that have spread to other parts of the body. It involves taking powerful medicines that kill cancerous cells. It does not cure thyroid cancer, but it may help to control the symptoms.
Thyroid Hormone Therapy– Radioactive iodine (RAI) is treatment for overactive thyroid cancer. The term “radioactive” may sound frightening, but it is a safe, generally well-tolerated, and reliable treatment that targets thyroid cells so there is little exposure to the rest of your body’s cells.
External Beam Radiation Therapy– It is use of manmade thyroid hormones to raise abnormally low levels of natural thyroid hormones in the body. Thyroid hormone is usually given in pill form and is often used to treat an underactive thyroid that is secreting little or no thyroid hormones.
Chemotherapy– It is rarely used to treat thyroid cancer, but it’s sometimes used to treat anplastic thyroid carcinomas that have spread to other parts of the body. It involves taking powerful medicines that kill cancerous cells. It does not cure thyroid cancer, but it may help to control the symptoms.
Tests and Procedures used to diagnose Thyroid Cancer include:
Blood test: A blood test called a thyroid function test is used to check the levels of thyroid hormones in your blood. Abnormal levels could mean that you have an overactive thyroid or an underactive thyroid, rather than cancer.
Ultrasound scan: An ultrasound scan uses sound waves to create an image of the inside of your body. An ultrasound scan of your neck can check for a lump in your thyroid that could be caused by cancer. If a potentially cancerous lump is found, a biopsy will be done to confirm the diagnosis.
Biopsy: The only way to confirm if a lump on the thyroid is cancer is to take a biopsy. This is where a small sample of cells are removed and studied under a microscope. A biopsy of the thyroid is usually done by inserting a thin needle into the lump. An ultrasound scan may be done at the same time to guide the needle into the right place. This is usually done as an outpatient procedure, which means you will not have to spend the night in hospital.
Further tests: The main tests used for this are:
- CT scan – A type of scan that uses a series of X-rays and a computer to create detailed images of the inside of the body.
- MRI scan – A type of scan that uses strong magnetic fields and radio waves to produce detailed images of the inside of the body.
Procedure for External-beam radiation therapy:
External-beam radiation therapy is a common treatment for thyroid cancer that has spread beyond the thyroid gland or for tumors that cannot be removed surgically. Here is an overview of the procedure for external-beam radiation therapy in thyroid cancer:
- Simulation: The first step is to determine the precise location of the tumor and the surrounding healthy tissue. This is done through a process called simulation, which involves using imaging techniques such as CT or MRI scans to create a detailed map of the area being treated.
- Treatment planning: Once the simulation is complete, the radiation oncologist will develop a treatment plan that outlines the dose and schedule of radiation. The goal is to deliver enough radiation to kill cancer cells while minimizing damage to healthy tissue.
- Radiation treatment: The actual radiation treatment involves the use of a machine called a linear accelerator. The machine delivers a high-energy beam of radiation to the tumor and surrounding tissue. The individual will lie on a treatment table and the machine will move around them to deliver radiation from different angles. Each treatment session typically lasts 15-30 minutes, and the total number of sessions will depend on the size and stage of the tumor.
- Follow-up: After radiation therapy, the individual will need to attend follow-up appointments to monitor their recovery and to ensure that the cancer does not return. Additional treatment, such as surgery or chemotherapy, may be necessary if the cancer has spread or if there is a high risk of recurrence.
Note:
It’s important to note that radiation therapy can cause side effects, such as fatigue, skin irritation, and changes in taste and smell. These side effects are usually temporary and can be managed with medication or other treatments. Your healthcare provider can provide more detailed information about the radiation therapy procedure and what to expect during recovery.
Procedure for Chemotherapy:
Chemotherapy is a less commonly used treatment for thyroid cancer, but it may be used in certain cases, such as when the cancer has spread to other parts of the body. Here is an overview of the procedure for chemotherapy in thyroid cancer.
- Drug administration: Chemotherapy drugs are usually administered intravenously (through a vein) or orally (in pill form). The drugs travel through the bloodstream to reach cancer cells throughout the body.
- Treatment schedule: The treatment schedule for chemotherapy varies depending on the type and stage of the cancer, as well as the individual’s overall health. Chemotherapy is usually given in cycles, with periods of treatment followed by periods of rest.
- Follow-up: After chemotherapy, the individual will need to attend follow-up appointments to monitor their recovery and to ensure that the cancer does not return. Additional treatment, such as surgery or radiation therapy, may be necessary if the cancer has not responded to chemotherapy or if there is a high risk of recurrence.
Note:
It’s important to note that chemotherapy can cause side effects, such as nausea, vomiting, hair loss, and fatigue. These side effects are usually temporary and can be managed with medication or other treatments. Your healthcare provider can provide more detailed information about the chemotherapy procedure and what to expect during recovery.
Procedure for Surgery:
Surgery is a common treatment for thyroid cancer, especially for early-stage cancers that are confined to the thyroid gland. The type of surgery will depend on the size and location of the tumor, as well as the individual’s overall health. Here is an overview of the procedure for surgery in thyroid cancer:
- Anesthesia: The individual will be given general anesthesia to ensure that they are asleep and pain-free during the procedure.
- Incision: The surgeon will make an incision in the neck to access the thyroid gland.
- Thyroid removal: The surgeon will remove all or part of the thyroid gland, depending on the size and stage of the tumor. This may involve removing one or both lobes of the thyroid gland.
- Lymph node removal: If the cancer has spread to nearby lymph nodes, the surgeon may also remove those lymph nodes during the surgery.
- Reconstruction: If the entire thyroid gland is removed, the individual will need to take thyroid hormone replacement medication for the rest of their life. If only part of the thyroid gland is removed, the remaining tissue may be able to produce enough thyroid hormone on its own.
- Closure: Once the thyroid gland and any affected lymph nodes have been removed, the surgeon will close the incision with sutures or staples.
- Follow-up: After surgery, the individual will need to attend follow-up appointments to monitor their recovery and to ensure that the cancer does not return. Additional treatment, such as radiation therapy or chemotherapy, may be necessary if the cancer has spread or if there is a high risk of recurrence.
Note:
It’s important to note that surgery for thyroid cancer can cause side effects, such as pain, swelling, and difficulty speaking or swallowing. These side effects are usually temporary and can be managed with medication or other treatments. Your healthcare provider can provide more detailed information about the surgery procedure and what to expect during recovery.
UTERINE CANCER
Disease Name: Uterine Cancer
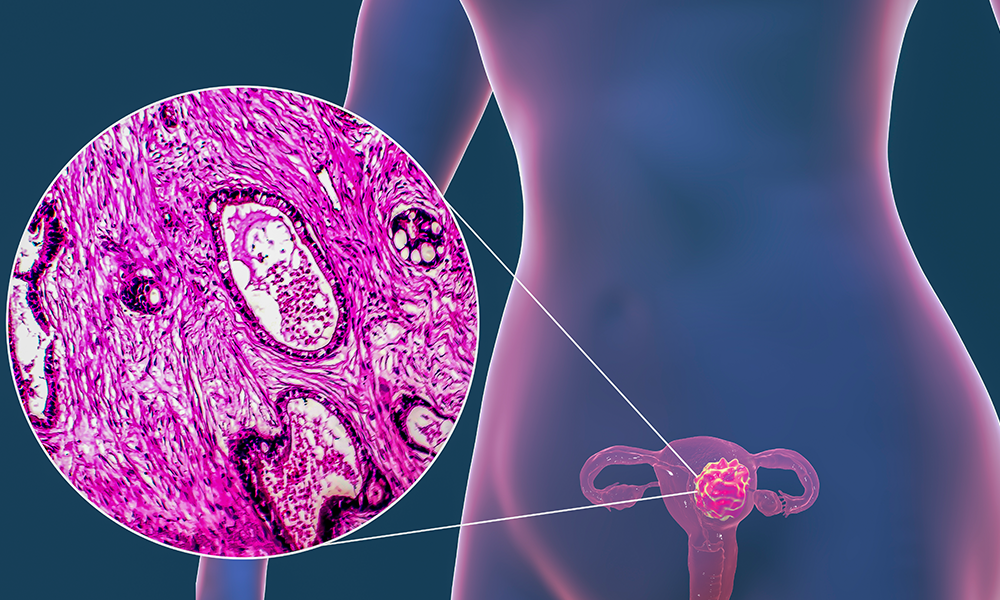
Uterine cancer is the most common cancer occurring within the female reproductive system. Uterine cancer begins when healthy cells in the uterus change and grow out of control, forming a mass called a tumor. A tumor can be cancerous or benign. A cancerous tumor is malignant, meaning it can grow and spread to other parts of the body. A benign tumor can grow but generally will not spread to other body parts.
The treatment for Uterine cancer depends on several factors, including the type and stage of the cancer, as well as the patient’s overall health. Treatment options for Uterine Cancer may include:
- Radiation Therapy
- Chemotherapy
- Hormone Therapy
- Immunotherapy
Radiation therapy- Radiation therapy is the use of high-energy x-rays or other particles to destroy cancer cells. A doctor who specializes in giving radiation therapy to treat cancer is called a radiation oncologist. External-beam radiation therapy uses a machine outside the body to deliver radiation to the pelvic region or the area designated by your radiation oncologist.
Chemotherapy- Chemotherapy is the use of drugs to destroy cancer cells, usually by keeping the cancer cells from growing, dividing, and making more cells. When recommended for endometrial cancer, chemotherapy usually is given after surgery. Chemotherapy is also considered if the endometrial cancer returns after the person’s initial treatment.
Hormone therapy- Hormone therapy is used to slow the growth of certain types of uterine cancer cells that have receptors to the hormones on them. These tumors are generally adenocarcinoma and are grade 1 or 2.
Immunotherapy- Immunotherapy uses the body’s natural defenses to fight cancer by improving your immune system’s ability to attack cancer cells.
In April 2021, the FDA approved the immunotherapy drug dostarlimab (Jemperli) to treat recurrent or advanced endometrial cancer with dMMR that has progressed either while on or after completing platinum-containing chemotherapy. Dostarlimab is given by vein every 3 weeks. Its most common side effects are fatigue, nausea, diarrhea, and constipation.
Tests and procedures used to diagnose Uterine Cancer include:
Your provider may perform one or more tests to confirm a diagnosis of uterine cancer:
Lab tests:
CA-125 assay is a blood draw that measures CA-125, a protein. A certain amount of CA-125 can point to cancer in your body.
Imaging tests:
CT scans take a series of detailed pictures of the inside of your body.
MRI scans use radio waves and a powerful magnet to create images.
Transvaginal ultrasound inserts a special probe (smooth, rounded device) into your vagina to get pictures of your uterus.
Other tests:
- Endometrial biopsy inserts a thin, flexible tube through your cervix (opening of your uterus) and into your uterus. Your provider removes a small amount of the endometrium.
- Hysteroscopy inserts a hysteroscope, a long thin tube, through your vagina and cervix to reach your uterus. This narrow instrument with a light and camera provides detailed images of your uterus.
- Dilation and curettage (D&C) is a more complex procedure to remove uterine tissue. It takes place in the operating room.
If you had a D&C or biopsy to remove tissue samples, your provider then sends the sample to a lab. There, a pathologist looks at the tissue to confirm if there’s cancer.
Procedure for Hormone Therapy:
Hormone therapy is a treatment option for some types of uterine cancer that are hormone-sensitive, meaning that they rely on hormones to grow. The procedure for hormone therapy in uterine cancer involves the following steps:
- Hormone receptor testing: Before hormone therapy can be prescribed, the cancer cells must be tested to determine whether they have receptors for estrogen and/or progesterone, which are hormones that can stimulate the growth of some uterine cancers.
- Hormone therapy drugs: If the cancer cells have estrogen and/or progesterone receptors, hormone therapy drugs may be prescribed to block the effects of these hormones or to lower their levels in the body. The most commonly used hormone therapy drugs for uterine cancer include selective estrogen receptor modulators (SERMs), aromatase inhibitors, and progestins.
- Treatment schedule: The treatment schedule for hormone therapy varies depending on the type and stage of the cancer, as well as the individual’s overall health. Hormone therapy may be given orally (in pill form) or through injection.
- Follow-up: After hormone therapy, the individual will need to attend follow-up appointments to monitor their response to treatment and to ensure that the cancer does not return. Additional treatment, such as surgery or radiation therapy, may be necessary if the cancer does not respond to hormone therapy or if there is a high risk of recurrence.
Note:
It’s important to note that hormone therapy can cause side effects, such as hot flashes, mood changes, and vaginal dryness. These side effects are usually temporary and can be managed with medication or other treatments. Your healthcare provider can provide more detailed information about the hormone therapy procedure and what to expect during treatment and recovery.
Procedure for Radiation Therapy:
Radiation therapy is a common treatment for uterine cancer, particularly for cases where the cancer has not spread beyond the uterus or nearby tissues. The procedure for radiation therapy in uterine cancer involves the following steps:
- Treatment planning: Before radiation therapy can begin, the individual will undergo imaging tests, such as CT scans or MRI scans, to determine the size and location of the tumor. Based on this information, the radiation oncologist will develop a treatment plan that outlines the dose and duration of radiation therapy.
- Radiation therapy sessions: Radiation therapy is typically given in multiple sessions over the course of several weeks. During each session, the individual will lie on a treatment table while a machine delivers high-energy radiation beams to the uterus and surrounding tissues. The radiation oncologist will ensure that the radiation is targeted to the tumor and that the surrounding healthy tissues are spared as much as possible.
- Follow-up: After radiation therapy, the individual will need to attend follow-up appointments to monitor their response to treatment and to ensure that the cancer does not return. Additional treatment, such as surgery or chemotherapy, may be necessary if the cancer does not respond to radiation therapy or if there is a high risk of recurrence.
Note:
It’s important to note that radiation therapy can cause side effects, such as fatigue, skin irritation, and bowel or bladder problems. These side effects are usually temporary and can be managed with medication or other treatments. Your healthcare provider can provide more detailed information about the radiation therapy procedure and what to expect during treatment and recovery.
Procedure for Chemotherapy:
Chemotherapy is a common treatment for uterine cancer, particularly for cases where the cancer has spread beyond the uterus or nearby tissues. The procedure for chemotherapy in uterine cancer involves the following steps:
- Treatment plan: Before chemotherapy can begin, the individual will undergo tests to determine the stage and extent of the cancer. Based on this information, the medical oncologist will develop a treatment plan that outlines the type and duration of chemotherapy drugs to be used.
- Chemotherapy sessions: Chemotherapy is typically given in cycles over the course of several months. The drugs are administered either intravenously (through a vein) or orally (in pill form). The frequency and duration of each cycle will depend on the individual’s overall health and the specific drugs being used.
- Follow-up: After chemotherapy, the individual will need to attend follow-up appointments to monitor their response to treatment and to ensure that the cancer does not return. Additional treatment, such as radiation therapy or surgery, may be necessary if the cancer does not respond to chemotherapy or if there is a high risk of recurrence.
Note:
It’s important to note that chemotherapy can cause side effects, such as nausea, hair loss, fatigue, and increased risk of infection. These side effects are usually temporary and can be managed with medication or other treatments. Your healthcare provider can provide more detailed information about the chemotherapy procedure and what to expect during treatment and recovery.
PANCREATIC CANCER
Disease name: Pancreatic Cancer
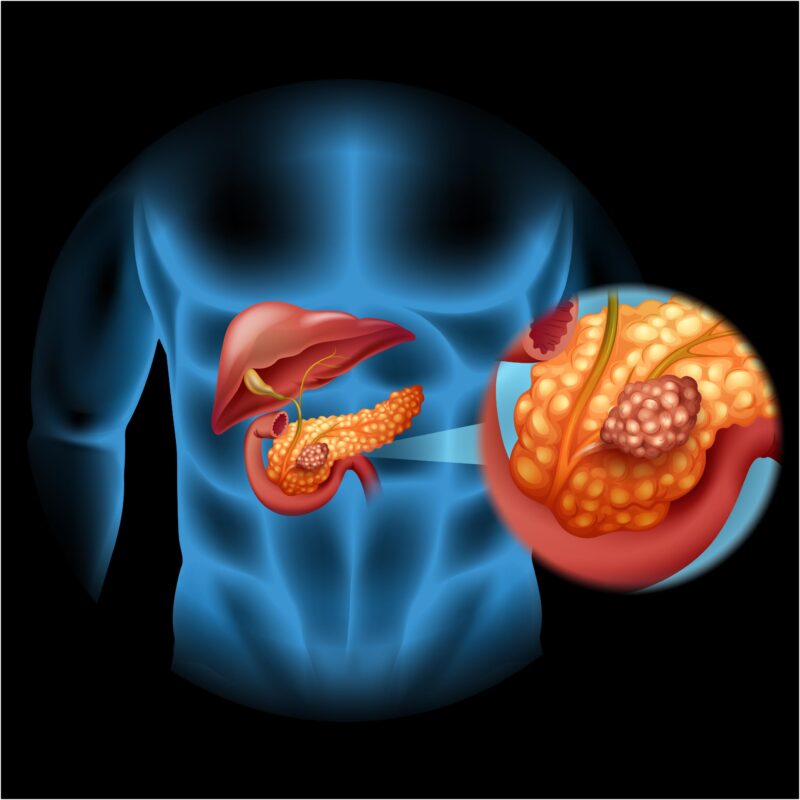
Pancreatic cancer is a type of cancer that occurs when abnormal cells grow uncontrollably in the pancreas. The pancreas is a gland located behind the stomach that produces enzymes to aid in digestion and hormones such as insulin to regulate blood sugar levels.
Pancreatic cancer is one of the deadliest types of cancer, as it often goes undetected until it has spread to other parts of the body. Symptoms may include abdominal pain, loss of appetite, weight loss, and jaundice. However, these symptoms can also be caused by other conditions, so it is important to see a doctor for proper diagnosis.
There are two main types of pancreatic cancer: exocrine tumors, which start in the cells that produce digestive enzymes, and endocrine tumors, which start in the cells that produce hormones. The most common type of pancreatic cancer is exocrine pancreatic cancer, which accounts for about 95% of cases.
Treatment for pancreatic cancer depends on the stage of the cancer and may include surgery, chemotherapy, radiation therapy, or a combination of these. However, even with treatment, the outlook for pancreatic cancer is often poor, with a five-year survival rate of around 10%.
Risk factors for pancreatic cancer include smoking, obesity, chronic pancreatitis, a family history of pancreatic cancer, and certain genetic conditions such as hereditary pancreatitis and Lynch syndrome. Making lifestyle changes such as quitting smoking, maintaining a healthy weight, and limiting alcohol intake may help reduce the risk of developing pancreatic cancer.
Treatments:
The treatment for pancreatic cancer depends on the stage of the cancer and the patient’s overall health. Treatment options may include:
- Surgery: Surgery is often the first treatment for pancreatic cancer, especially if the cancer has not spread to other parts of the body. The surgeon may remove the tumor and a portion of the pancreas, or in more advanced cases, may remove the entire pancreas and nearby organs.
- Chemotherapy: Chemotherapy uses drugs to kill cancer cells. It is often used in combination with surgery or radiation therapy. Chemotherapy may also be used to help control the growth of the cancer if it has spread to other parts of the body.
- Radiation therapy: Radiation therapy uses high-energy X-rays or other types of radiation to kill cancer cells. It may be used in combination with surgery or chemotherapy, or as a palliative treatment to help relieve pain and other symptoms.
- Targeted therapy: Targeted therapy uses drugs that target specific proteins or genes that contribute to the growth and spread of cancer cells. It may be used in combination with chemotherapy or other treatments.
- Immunotherapy: Immunotherapy uses drugs to stimulate the immune system to recognize and attack cancer cells. It may be used in combination with other treatments or as a stand-alone treatment for some types of pancreatic cancer.
It is important to note that not all patients are eligible for every treatment option, and the decision on the best course of treatment depends on various factors, such as the stage and location of the cancer, the patient’s overall health and medical history, and their preferences.
Tests and Procedures to diagnose pancreatic cancer:
There are several tests and procedures that may be used to diagnose pancreatic cancer. These include:
- Imaging tests: Imaging tests, such as computed tomography (CT) scans, magnetic resonance imaging (MRI) scans, and positron emission tomography (PET) scans, can provide detailed images of the pancreas and surrounding tissues. These tests can help identify abnormalities in the pancreas, such as tumors.
- Endoscopic ultrasound (EUS): EUS is a procedure in which an ultrasound probe is inserted into the digestive tract via an endoscope. This allows the doctor to obtain detailed images of the pancreas and surrounding tissues, and to take samples of abnormal tissue for further testing.
- Biopsy: A biopsy involves taking a small sample of tissue from the pancreas to examine under a microscope. This can be done using a needle inserted through the skin or during an endoscopic procedure.
- Blood tests: Blood tests can help detect certain substances, such as tumor markers or enzymes produced by the pancreas, that may be indicative of pancreatic cancer.
- Laparoscopy: In some cases, a laparoscopy may be used to examine the pancreas and surrounding tissues. This involves inserting a thin, lighted tube with a camera through a small incision in the abdomen.
It’s important to note that the best diagnostic approach for pancreatic cancer depends on various factors, such as the patient’s symptoms, medical history, and overall health. A doctor may use one or more of these tests to confirm the diagnosis of pancreatic cancer and to determine the stage of the cancer.
Medications:
There are several medications that may be used to treat pancreatic cancer. The choice of medication depends on the stage and type of cancer, as well as the patient’s overall health and medical history. Some medications that may be used to treat pancreatic cancer include:
- Chemotherapy drugs: Chemotherapy drugs are often used to treat pancreatic cancer. They work by killing rapidly dividing cancer cells. Some commonly used chemotherapy drugs for pancreatic cancer include gemcitabine, nab-paclitaxel, fluorouracil, and irinotecan.
- Targeted therapy drugs: Targeted therapy drugs work by targeting specific molecules or pathways that contribute to the growth and spread of cancer cells. For example, erlotinib is a targeted therapy drug that targets the epidermal growth factor receptor (EGFR) and is used in combination with gemcitabine to treat pancreatic cancer.
- Immunotherapy drugs: Immunotherapy drugs work by stimulating the immune system to recognize and attack cancer cells. For example, pembrolizumab is an immunotherapy drug that targets the programmed cell death protein 1 (PD-1) pathway and may be used to treat some types of pancreatic cancer.
- Pain medications: Pancreatic cancer can cause significant pain. Pain medications, such as opioids and nonsteroidal anti-inflammatory drugs (NSAIDs), may be used to help manage pain.
- Palliative care medications: Palliative care medications, such as antiemetics and laxatives, may be used to manage symptoms such as nausea, vomiting, and constipation in patients with pancreatic cancer.
It’s important to note that not all patients are eligible for every medication, and the choice of medication depends on various factors, such as the stage and location of the cancer, the patient’s overall health and medical history, and their preferences.
Procedure for Surgery:
The specific procedure for surgery for pancreatic cancer depends on the location and stage of the cancer, as well as the patient’s overall health and medical history. The most common surgical procedures for pancreatic cancer include:
- Whipple procedure (pancreaticoduodenectomy): This is the most common surgery for pancreatic cancer, especially if the tumor is located in the head of the pancreas. During a Whipple procedure, the surgeon removes the head of the pancreas, as well as the duodenum (the first part of the small intestine), part of the stomach, the gallbladder, and the bile ducts. The remaining parts of the pancreas are then connected to the remaining digestive organs.
- Distal pancreatectomy: This surgery is used to remove tumors located in the body or tail of the pancreas. During a distal pancreatectomy, the surgeon removes the body and/or tail of the pancreas, as well as the spleen, if necessary.
- Total pancreatectomy: In some cases, a total pancreatectomy may be necessary if the cancer has spread throughout the pancreas. During this procedure, the entire pancreas, as well as the spleen, gallbladder, and parts of the stomach and small intestine, are removed. The patient will need to take pancreatic enzyme supplements and insulin injections for the rest of their life after this procedure.
Surgery for pancreatic cancer is a major procedure and can be associated with significant risks and complications, such as bleeding, infection, and problems with digestion. Recovery from surgery may also be challenging, and patients may need to spend several days or weeks in the hospital after the procedure. It’s important to discuss the risks and benefits of surgery with a healthcare provider to determine the best treatment approach for pancreatic cancer.
Procedure for Chemotherapy:
Chemotherapy is a common treatment for pancreatic cancer and involves the use of drugs to kill cancer cells. The specific procedure for chemotherapy for pancreatic cancer may vary depending on the type and stage of cancer, as well as the patient’s overall health and medical history. Here is a general overview of the procedure for chemotherapy in pancreatic cancer:
- Administration of chemotherapy drugs: Chemotherapy drugs can be given in different ways, including intravenously (IV) through a vein in the arm or through a catheter placed in a large vein, or orally in the form of pills or capsules. The drugs are usually given in cycles, with a period of treatment followed by a period of rest.
- Frequency of treatment: The frequency of chemotherapy treatment may vary depending on the type of chemotherapy drugs used and the stage of the cancer. Chemotherapy may be given once a week or every two or three weeks.
- Duration of treatment: The duration of chemotherapy treatment for pancreatic cancer may also vary depending on the type of cancer and the response to treatment. Treatment may last for several months or longer.
- Monitoring of side effects: Chemotherapy drugs can cause side effects, such as nausea, vomiting, fatigue, hair loss, and increased risk of infection. Patients undergoing chemotherapy will be closely monitored for side effects and may receive medication to manage them.
- Response to treatment: Patients undergoing chemotherapy for pancreatic cancer will be closely monitored to assess the response to treatment. Imaging tests, such as CT scans and MRIs, may be used to evaluate the size of the tumor and whether it is shrinking or growing.
It’s important to note that the specific procedure for chemotherapy for pancreatic cancer may vary depending on individual patient factors, and it’s important to discuss the best treatment options with a healthcare provider.
Procedure for Targeted Therapy:
Targeted therapy is a type of cancer treatment that uses drugs to specifically target cancer cells while minimizing damage to normal cells. Targeted therapy drugs work by blocking the growth and spread of cancer cells by targeting specific proteins or other molecules that are involved in the growth and survival of cancer cells.
Here is a general procedure for targeted therapy in pancreatic cancer:
- Diagnosis and Molecular Profiling: To determine if a patient is a candidate for targeted therapy, the patient will need to undergo diagnosis and molecular profiling. This includes imaging tests like CT or MRI scans, as well as laboratory tests like a biopsy or blood tests to determine the specific genetic mutations or alterations that are present in the cancer cells.
- Identifying Targeted Therapy Options: Based on the molecular profiling results, the oncologist will identify potential targeted therapy options that are specific to the genetic mutations or alterations present in the cancer cells. There are several targeted therapy drugs that have been approved for pancreatic cancer, including erlotinib, gemcitabine, and nab-paclitaxel.
- Treatment Plan: Once the targeted therapy options have been identified, the oncologist will work with the patient to develop a treatment plan. This may involve using targeted therapy alone or in combination with other treatments like chemotherapy, radiation therapy, or surgery.
- Treatment Monitoring: During treatment, the patient will undergo regular imaging tests and laboratory tests to monitor the effectiveness of the targeted therapy. The oncologist may adjust the treatment plan as needed based on how the cancer is responding.
- Side Effect Management: Targeted therapy drugs can have side effects, and the oncologist will work with the patient to manage any side effects that occur during treatment.
It is important to note that targeted therapy may not be suitable for all patients with pancreatic cancer, and the effectiveness of targeted therapy can vary depending on the specific genetic mutations or alterations present in the cancer cells. Patients should discuss their individual treatment options with their oncologist to determine the best course of treatment for their specific case.
CERVICAL CANCER
Disease name: Cervical Cancer
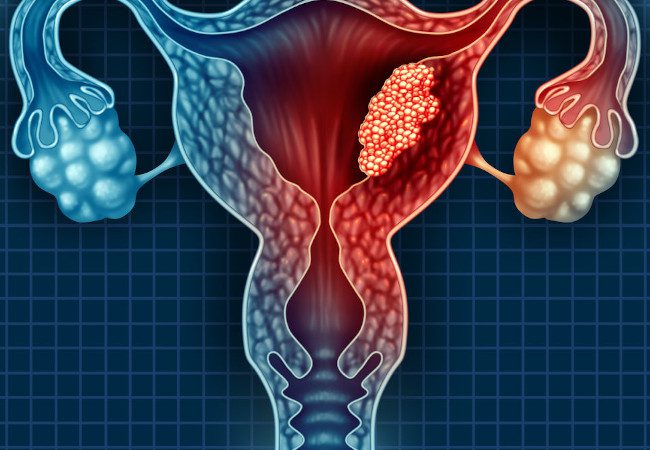
Cervical cancer is a type of cancer that develops in the cervix, which is the lower part of the uterus that connects to the vagina. It is usually caused by the human papillomavirus (HPV), which is a common sexually transmitted infection.
Cervical cancer can be classified into two main types: squamous cell carcinoma, which accounts for about 80% of cases, and adenocarcinoma, which accounts for about 15-20% of cases. Other less common types of cervical cancer include adenosquamous carcinoma and small cell carcinoma.
Symptoms of cervical cancer may include abnormal vaginal bleeding, such as bleeding after sex or between periods, pelvic pain, pain during sex, and vaginal discharge that may be tinged with blood.
Cervical cancer can be diagnosed through a variety of methods, including a Pap smear, HPV test, colposcopy, and biopsy. Treatment options for cervical cancer depend on the stage and location of the cancer, as well as the patient’s overall health. Treatment may include surgery, radiation therapy, chemotherapy, or a combination of these approaches.
Prevention of cervical cancer includes getting vaccinated against HPV, practicing safe sex, and getting regular Pap smears and HPV tests. Early detection through regular screenings is important for improving outcomes and reducing the risk of complications associated with cervical cancer.
Treatments:
The treatment for cervical cancer depends on several factors, including the stage of the cancer, the size and location of the tumor, and the patient’s overall health. The main treatment options for cervical cancer include:
- Surgery: Surgery is the main treatment for early-stage cervical cancer. The type of surgery depends on the size and location of the tumor. A cone biopsy or loop electrosurgical excision procedure (LEEP) may be done to remove small tumors. For larger tumors, a radical hysterectomy, which involves removing the uterus, cervix, and surrounding tissues, may be recommended.
- Radiation therapy: Radiation therapy uses high-energy X-rays to kill cancer cells. It may be used alone or in combination with surgery or chemotherapy. External beam radiation therapy is directed at the pelvic region, while brachytherapy involves placing a radioactive source inside the vagina to target the cancer cells.
- Chemotherapy: Chemotherapy uses drugs to kill cancer cells. It may be given before or after surgery, or in combination with radiation therapy. Chemotherapy can also be used to treat advanced or recurrent cervical cancer.
- Targeted therapy: Targeted therapy drugs can target specific proteins or genes that are involved in the growth and spread of cancer cells. Bevacizumab is a targeted therapy drug that has been approved for the treatment of advanced cervical cancer.
The choice of treatment depends on the individual case, and treatment plans are often tailored to the patient’s specific needs. In some cases, a combination of treatments may be used. It is important to discuss the potential benefits and risks of each treatment option with a healthcare provider.
Tests and Procedures to diagnose cervical cancer:
There are several tests and procedures that can be used to diagnose cervical cancer, including:
- Pap smear: A Pap smear is a screening test used to detect abnormal cells in the cervix. During the test, a healthcare provider will collect a sample of cells from the cervix and send it to a laboratory for analysis.
- HPV test: An HPV test is used to detect the presence of the human papillomavirus (HPV), which is the primary cause of cervical cancer. The test may be performed at the same time as a Pap smear.
- Colposcopy: A colposcopy is a procedure that uses a special instrument called a colposcope to examine the cervix for abnormal cells. During the procedure, a healthcare provider may take a biopsy of any abnormal areas for further analysis.
- Biopsy: A biopsy involves removing a small sample of tissue from the cervix for examination under a microscope. This can help determine if cancer is present and what type it is.
- Imaging tests: Imaging tests such as a CT scan, MRI, or PET scan may be used to determine the size and location of the cancer, and whether it has spread to other parts of the body.
It’s important for women to undergo regular Pap smears and HPV tests to detect any abnormal changes in the cervix early on, before they develop into cancer. If abnormal cells are found, further testing and evaluation may be needed to determine if cancer is present and what the best course of treatment may be.
Medications:
The main treatments for cervical cancer are surgery, radiation therapy, and chemotherapy. However, there are some medications that may be used to treat cervical cancer or manage its symptoms. These include:
- Bevacizumab: Bevacizumab is a targeted therapy drug that works by blocking the growth of blood vessels that supply nutrients to cancer cells. It has been approved for the treatment of advanced cervical cancer.
- Cisplatin: Cisplatin is a chemotherapy drug that is often used in combination with radiation therapy to treat cervical cancer. It works by interfering with the DNA of cancer cells, preventing them from dividing and growing.
- Paclitaxel: Paclitaxel is another chemotherapy drug that is sometimes used to treat cervical cancer. It works by preventing cancer cells from dividing and growing.
- Pain medications: Pain medications, such as opioids or nonsteroidal anti-inflammatory drugs (NSAIDs), may be used to manage pain associated with cervical cancer or its treatment.
- Hormone therapy: Hormone therapy may be used to treat advanced cervical cancer that has spread to other parts of the body. Hormone therapy drugs work by blocking the production of estrogen, which can stimulate the growth of some types of cervical cancer.
It’s important to note that the specific medications used to treat cervical cancer may vary depending on the stage of the cancer, the patient’s overall health, and other factors. Treatment plans are often tailored to the individual case, and it’s important to discuss the potential benefits and risks of each treatment option with a healthcare provider.
Procedure for Radiation Therapy:
Radiation therapy is a common treatment option for cervical cancer, especially for locally advanced or recurrent disease. The procedure for radiation therapy in cervical cancer typically involves the following steps:
- Simulation: Before radiation therapy begins, a simulation is done to determine the exact location and size of the cancer, as well as the surrounding healthy tissues. This may involve taking CT scans, MRI or PET scans, or using X-rays to create a 3D image of the area to be treated.
- Planning: Once the simulation is complete, a team of radiation oncologists and medical physicists will work together to create a treatment plan. The plan will specify the exact dose of radiation, the number of treatments, and the angle at which the radiation will be delivered.
- Treatment: During radiation therapy, the patient lies on a table while a machine delivers high-energy X-rays or other types of radiation to the area around the cervix. The procedure is usually painless, but the patient may need to be immobilized with a mask or other device to ensure that they remain still during the treatment.
- Follow-up: After radiation therapy is complete, the patient will be monitored closely for any side effects or complications. They may need additional tests, such as imaging scans or blood tests, to determine how well the treatment worked.
It’s important for patients undergoing radiation therapy to follow their healthcare provider’s instructions carefully, and to report any side effects or concerns right away. Side effects of radiation therapy may include fatigue, nausea, diarrhea, skin irritation, and vaginal dryness or discharge. In some cases, radiation therapy may also cause long-term side effects, such as scarring or damage to nearby organs.
Procedure for Chemotherapy:
hemotherapy is a common treatment option for cervical cancer, especially for advanced or metastatic disease. The procedure for chemotherapy in cervical cancer typically involves the following steps:
- Drug selection: A combination of chemotherapy drugs is usually used to treat cervical cancer. The specific drugs used may vary depending on the stage of the cancer, the patient’s overall health, and other factors. Common drugs used in cervical cancer chemotherapy include cisplatin, paclitaxel, and topotecan.
- Administration: Chemotherapy drugs are usually given intravenously (through a vein) in cycles, with a period of rest between each cycle to allow the body to recover. Depending on the drugs used, chemotherapy may be given in an outpatient setting or in the hospital.
- Follow-up: After chemotherapy is complete, the patient will be monitored closely for any side effects or complications. They may need additional tests, such as imaging scans or blood tests, to determine how well the treatment worked.
It’s important for patients undergoing chemotherapy to follow their healthcare provider’s instructions carefully, and to report any side effects or concerns right away. Side effects of chemotherapy may include nausea, vomiting, hair loss, fatigue, and an increased risk of infection. In some cases, chemotherapy may also cause long-term side effects, such as nerve damage or kidney damage.
Procedure for Targeted Therapy:
Targeted therapy is a newer treatment approach that uses drugs or other substances to target specific molecules or pathways that contribute to cancer growth. While targeted therapy drugs are not yet widely used for cervical cancer, ongoing research is exploring their potential in this area. The procedure for targeted therapy in cervical cancer may involve the following steps:
- Biomarker testing: Before targeted therapy can be used, a patient’s tumor tissue must be tested for specific biomarkers or genetic mutations that may make the cancer more responsive to targeted therapy. This may involve genetic testing or other types of molecular testing.
- Drug selection: Based on the results of the biomarker testing, a healthcare provider may recommend a targeted therapy drug that is designed to specifically target the identified molecular pathway. Examples of targeted therapy drugs that may be used for cervical cancer include bevacizumab, which targets a molecule called VEGF that is involved in blood vessel formation, and pembrolizumab, which targets the PD-1 protein to help the immune system recognize and attack cancer cells.
- Administration: Targeted therapy drugs are usually given intravenously (through a vein) in cycles, with a period of rest between each cycle to allow the body to recover. Depending on the drug used, targeted therapy may be given in an outpatient setting or in the hospital.
- Follow-up: After targeted therapy is complete, the patient will be monitored closely for any side effects or complications. They may need additional tests, such as imaging scans or blood tests, to determine how well the treatment worked.
It’s important for patients undergoing targeted therapy to follow their healthcare provider’s instructions carefully, and to report any side effects or concerns right away. Side effects of targeted therapy may include fatigue, nausea, skin rash, and an increased risk of infection. In some cases, targeted therapy may also cause long-term side effects, such as organ damage or hormone imbalances.
OVARIAN CANCER
Disease Name: Ovarian Cancer
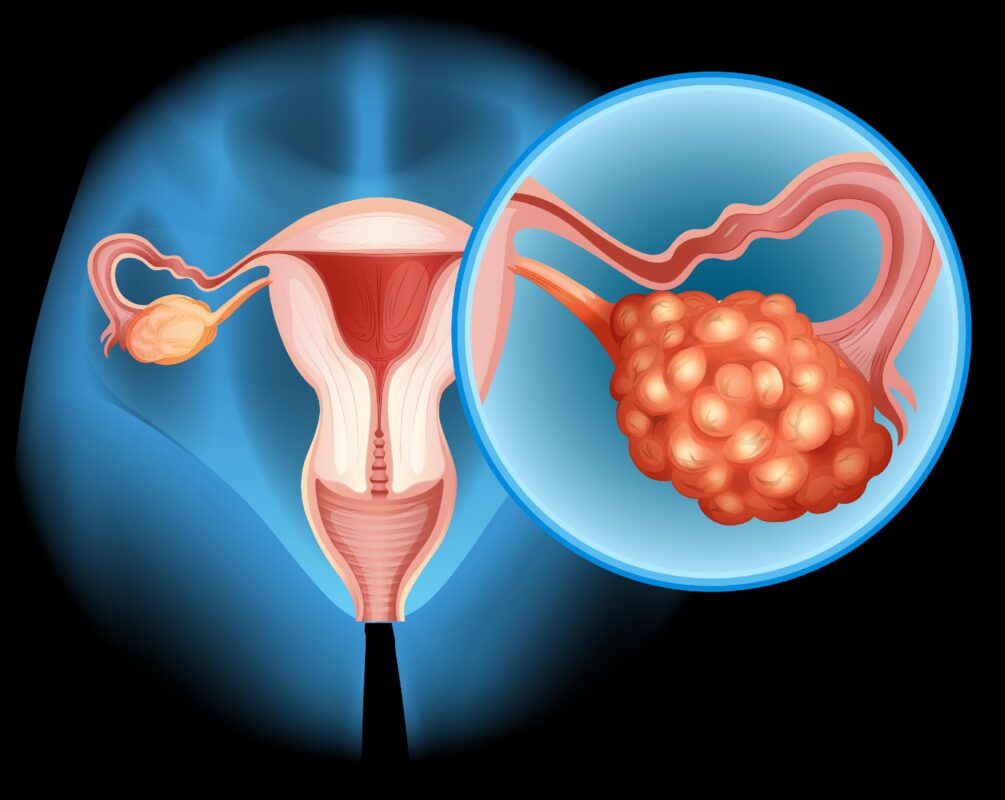
Ovarian cancer is a type of cancer that originates in the ovaries, which are the female reproductive organs responsible for producing eggs. It is the fifth most common cancer in women and the most lethal gynecologic cancer, causing more deaths than any other cancer of the female reproductive system.
Ovarian cancer is often referred to as the “silent killer” because it often goes undetected until it has spread beyond the ovaries, making it more difficult to treat. Symptoms of ovarian cancer can be vague and nonspecific, and may include bloating, abdominal pain or swelling, loss of appetite, and changes in bowel or bladder habits.
There are several types of ovarian cancer, including epithelial, germ cell, and stromal tumors. Epithelial tumors are the most common type and develop from the cells that cover the surface of the ovary. Germ cell and stromal tumors are less common and develop from the cells that produce eggs and hormones, respectively.
Treatment for ovarian cancer typically involves a combination of surgery, chemotherapy, and, in some cases, radiation therapy. The specific treatment plan will depend on several factors, including the stage of the cancer, the patient’s overall health, and the type of ovarian cancer.
Early detection and diagnosis are key to improving outcomes for women with ovarian cancer. Women who are at higher risk for ovarian cancer, such as those with a family history of the disease, may be advised to undergo regular screenings or genetic testing to identify potential risk factors.
Treatments:
The treatment for ovarian cancer depends on the type of ovarian cancer, stage of the cancer, and the patient’s overall health. Treatment options may include one or a combination of the following:
- Surgery: Surgery is the main treatment for ovarian cancer. The goal of surgery is to remove as much of the tumor as possible. Depending on the stage of the cancer, surgery may involve removing the affected ovary, the fallopian tubes, and the uterus (hysterectomy) along with the removal of nearby lymph nodes and other tissues.
- Chemotherapy: Chemotherapy uses drugs to kill cancer cells. It is often used in combination with surgery and may be given before or after surgery. Chemotherapy is typically administered intravenously, but may also be given as a pill.
- Targeted therapy: Targeted therapy uses drugs to specifically target cancer cells while minimizing damage to healthy cells. Targeted therapy drugs may be used in combination with chemotherapy or as a standalone treatment for certain types of ovarian cancer.
- Radiation therapy: Radiation therapy uses high-energy beams to kill cancer cells. It is not commonly used for ovarian cancer, but may be used in some cases.
In addition to these treatments, other supportive care options may also be used to help manage symptoms and improve quality of life for ovarian cancer patients. These may include pain management, nutritional support, and counseling.
It is important for patients with ovarian cancer to work closely with their healthcare team to develop an individualized treatment plan that takes into account their specific circumstances and goals. Early detection and treatment are key to improving outcomes for women with ovarian cancer.
Tests and Procedures to diagnose ovarian cancer:
There are several tests and procedures used to diagnose ovarian cancer. These may include:
- Pelvic exam: A pelvic exam involves a physical examination of the ovaries, uterus, and other pelvic organs to check for any abnormalities or signs of cancer.
- Imaging tests: Imaging tests, such as ultrasound, CT scan, or MRI, may be used to produce detailed images of the ovaries and surrounding tissues to help detect any abnormalities.
- Blood tests: Blood tests, such as the CA-125 test, may be used to measure levels of certain proteins that are often elevated in women with ovarian cancer. However, the CA-125 test is not always reliable for diagnosing ovarian cancer, as it can be elevated for other reasons, such as menstruation, pregnancy, or other medical conditions.
- Biopsy: A biopsy involves the removal of a tissue sample from the ovary for examination under a microscope to determine if cancer cells are present. Biopsies may be performed during surgery or using a needle inserted through the skin and into the ovary (a procedure called a needle biopsy).
- Genetic testing: Genetic testing may be recommended for women with a family history of ovarian or breast cancer to check for genetic mutations that increase the risk of developing ovarian cancer.
It is important to note that no single test can definitively diagnose ovarian cancer. A combination of tests and procedures may be used to make a diagnosis and determine the stage and extent of the cancer. Women who experience symptoms such as bloating, abdominal pain or swelling, loss of appetite, or changes in bowel or bladder habits should speak with their healthcare provider about the need for further testing.
Medications:
There are several medications used to treat ovarian cancer. These may include:
- Chemotherapy drugs: Chemotherapy drugs are the most common medications used to treat ovarian cancer. They work by killing rapidly dividing cancer cells. Chemotherapy may be given before or after surgery, depending on the stage of the cancer. Some common chemotherapy drugs used to treat ovarian cancer include carboplatin, paclitaxel, and cisplatin.
- Targeted therapy drugs: Targeted therapy drugs are designed to target specific proteins or genes in cancer cells. These drugs may be used in combination with chemotherapy or as a standalone treatment for certain types of ovarian cancer. Some targeted therapy drugs used to treat ovarian cancer include bevacizumab, olaparib, and rucaparib.
- Hormone therapy drugs: Hormone therapy drugs work by blocking the effects of certain hormones, such as estrogen, that can stimulate the growth of some types of ovarian cancer. Hormone therapy is typically used to treat stromal tumors, which are a type of ovarian cancer that develops from the cells that produce hormones. Some hormone therapy drugs used to treat ovarian cancer include letrozole and tamoxifen.
- Immunotherapy drugs: Immunotherapy drugs work by stimulating the immune system to attack cancer cells. They may be used to treat some types of ovarian cancer, such as germ cell tumors. Some immunotherapy drugs used to treat ovarian cancer include pembrolizumab and nivolumab.
It is important to note that the specific medication(s) used to treat ovarian cancer will depend on several factors, including the stage of the cancer, the type of ovarian cancer, and the patient’s overall health. Treatment may involve a combination of medications and other therapies, and may be adjusted as needed based on how well the cancer responds to treatment.
Procedure for Surgery:
Surgery is a common treatment option for ovarian cancer, and the specific procedure will depend on several factors, including the stage and extent of the cancer. The main types of surgery used to treat ovarian cancer include:
- Total hysterectomy: This procedure involves the removal of the uterus and cervix, as well as the ovaries and fallopian tubes. This is typically recommended for women with early-stage ovarian cancer who have not yet gone through menopause.
- Bilateral salpingo-oophorectomy: This procedure involves the removal of both ovaries and fallopian tubes. This may be recommended for women with early-stage ovarian cancer who have completed childbearing, or for women at high risk of developing ovarian cancer due to genetic mutations.
- Omentectomy: This procedure involves the removal of the omentum, a layer of fatty tissue that covers the abdominal organs. This may be recommended for women with more advanced ovarian cancer to remove any cancerous tissue that has spread to the omentum.
- Lymph node dissection: This procedure involves the removal of lymph nodes in the pelvis and abdomen to check for any cancerous cells that may have spread beyond the ovaries.
- Debulking surgery: This procedure involves the removal of as much cancerous tissue as possible, which may involve the removal of other organs or tissues in the pelvis or abdomen.
Surgery is typically performed under general anesthesia and may involve a laparoscopic or open approach. Recovery time and potential complications will depend on the specific procedure and the patient’s overall health.
Procedure for Chemotherapy:
Chemotherapy is a common treatment option for ovarian cancer and is typically given after surgery to remove as much cancer as possible. The specific chemotherapy regimen used will depend on several factors, including the stage and type of ovarian cancer. Chemotherapy drugs are usually administered intravenously, but may also be given orally.
The chemotherapy drugs used for ovarian cancer are usually given in cycles, with a period of treatment followed by a rest period. The length and number of cycles will depend on the individual patient’s situation. Some common chemotherapy drugs used to treat ovarian cancer include:
- Carboplatin: This is a platinum-based chemotherapy drug that is often used in combination with paclitaxel.
- Paclitaxel: This is a taxane-based chemotherapy drug that is often used in combination with carboplatin.
- Cisplatin: This is another platinum-based chemotherapy drug that may be used in combination with other drugs.
- Doxorubicin: This is an anthracycline-based chemotherapy drug that may be used in combination with other drugs.
- Topotecan: This is a topoisomerase inhibitor chemotherapy drug that may be used to treat recurrent ovarian cancer.
Chemotherapy can cause side effects, including fatigue, hair loss, nausea, vomiting, and an increased risk of infection. These side effects can usually be managed with medications or other supportive measures. The specific side effects and management strategies will depend on the individual patient and the chemotherapy drugs used.
Procedure for Targeted Therapy:
Targeted therapy is a type of cancer treatment that specifically targets certain proteins or molecules that are involved in the growth and spread of cancer cells. Targeted therapy may be used alone or in combination with chemotherapy to treat ovarian cancer. The specific targeted therapy used will depend on the patient’s individual situation, including the stage and type of ovarian cancer.
Some common targeted therapies used to treat ovarian cancer include:
- PARP inhibitors: These drugs target the PARP enzyme, which is involved in repairing damaged DNA. Inhibiting this enzyme can cause cancer cells to die. Olaparib, niraparib, and rucaparib are PARP inhibitors that have been approved for the treatment of ovarian cancer.
- Bevacizumab: This drug targets a protein called vascular endothelial growth factor (VEGF), which promotes the growth of blood vessels that supply oxygen and nutrients to cancer cells. Bevacizumab can help to slow the growth and spread of ovarian cancer cells.
- Antibody-drug conjugates: These drugs combine an antibody that targets a specific protein on cancer cells with a chemotherapy drug. This allows the chemotherapy drug to be delivered directly to the cancer cells while minimizing damage to healthy cells. Trastuzumab deruxtecan is an antibody-drug conjugate that has shown promise in the treatment of ovarian cancer.
Targeted therapy can cause side effects, which can vary depending on the specific drug used. Some common side effects include fatigue, nausea, diarrhea, and skin rashes. These side effects can usually be managed with medications or other supportive measures. The specific side effects and management strategies will depend on the individual patient and the targeted therapy used.
ALLOPATHY CENTERS IN ANDHRA PRADESH AND TELANGANA
- Cancer Clinics- Cancer Hospital in Hyderabad – Jubilee Hills
Address: Plot No. 573/I, 1 st Floor, Park View Building, Road No. 1, Jubilee Hills, Hyderabad, Telangana 500033
- PACE Hospitals – Hitech City
Address: Metro Pillar Number C1775, 18, Hitech City Rd, HUDA Techno Enclave, HITEC City, Hyderabad, Telangana 500081
- Apollo Cancer Centre, Hyderabad
Address: 8-2-293/82/J-III, 553/1, Road No. 92, Jubilee Hills, Hyderabad, Telangana 500033
- Onco Cancer Centre, Gachibowli, Hyderabad
Address: 4th Floor, Adilakshmi Square (above Pi International Plot no. 137 & 12, Old Mumbai Hwy, Gachibowli, Hyderabad, Telangana 500032
- Yashoda Cancer Hospital
Address: 16-10-29, Nallakunta Cross Road, Malakpet, Hyderabad, Telangana 500036
- Mahatma Gandhi Cancer Hospital & Research Institute
Address: Plot No:1, Sector:7, MVP Colony, Visakhapatnam, Andhra Pradesh 530017
- HCG CANCER CENTER VIZAG
Address: Pinnacle Hospital Compound, APIIC Health City, Arilova, Chinnagadili, Andhra Pradesh 530040
- American Oncology Institute (Cancer Hospital) – Vijayawada
Address: 6-224/2, At NRI Hospital, Mangalagiri, Chinakakani, Andhra Pradesh 522503
- HCG CURIE CITY CANCER CENTRE
Address: #44-1-1/3, Padavalarevu, Gunadala, Vijayawada, Andhra Pradesh 520004
- Vrindaa Hospitals | Best Cancer treatment in Vizag
Address: Plot No.14E,Health City, Arilova, Visakhapatnam, Andhra Pradesh 530040
AYURVEDIC HOSPITALS AND ORGANISATIONS
- Shalini Ayurveda Hospital
Address: 30-93-6 Kanithi High school Road Near Appikonda Seven Temples center Kanithi RH colony, Vadlapudi, Visakhapatnam, Andhra Pradesh 530046
- Travancore Ayurveda NABH Panchakarma Clinic | MVP Colony | Vizag
Address: Plot No 111/3,MIG -1 Near Mahatma Gandhi Cancer Hospital, Sector 3, MVP Colony, Visakhapatnam, Andhra Pradesh 530017
- sri vemayaswamy ayurvedic hospital
Address: GWGV+M7G, Cholla veedu, Andhra Pradesh 523372
- Seetharama Ayurvedic Hospital & Panchakarma Centre
Address: Old, Rainbow hospital line, near Vijaya diagnosis center, N R Peta, Kurnool, Andhra Pradesh 518004
- Sri Venkata Sai Ayurvedic & Panchakarma Hospital
Address: near Bank of Maharashtra, Venkata Ramana Colony, Teachers Colony, Kurnool, Andhra Pradesh 518005