Diabetes Center
Diabetic ketoacidosis, Insulin lispro (Humalog), Insulin aspart (NovoLog), Insulin glulisine (Apidra), Insulin glargine (Lantus), Insulin detemir (Levemir), Insulin degludec (Tresiba), Pramlintide (Symlin), Metformin, GLP-1 receptor agonists, Exenatide (Byetta) Liraglutide (Victoza), Aspirin.
Type 1 Diabetes
What is Type 1 Diabetes
Type 1 diabetes is a chronic condition that occurs when the pancreas produces little or no insulin, which is a hormone that regulates blood sugar levels. As a result, people with type 1 diabetes require insulin therapy to manage their blood sugar levels.

Doctors often diagnose type 1 diabetes in children and young adults when they have diabetes symptoms, such as feeling thirsty and having to urinate more often, or if they may have diabetic ketoacidosis. Symptoms in adults may be less specific.
Type 1 diabetes can run in families. A study called TrialNet offers free testing to relatives of people with type 1 diabetes, even if the relatives don’t have symptoms.
Medications
There are several types of insulin therapy available for people with type 1 diabetes, including
- Rapid-acting insulin: This type of insulin starts working within 15 minutes of injection and peaks in about an hour. Examples include insulin lispro (Humalog), insulin aspart (NovoLog), and insulin glulisine (Apidra).
- Short-acting insulin: This type of insulin starts working within 30 minutes of injection and peaks in 2 to 3 hours. Regular insulin (Humulin R, Novolin R) is an example.
- Intermediate-acting insulin: This type of insulin takes longer to start working (2 to 4 hours after injection) and peaks in 4 to 12 hours. Examples include NPH insulin (Humulin N, Novolin N).
- Long-acting insulin: This type of insulin starts working several hours after injection and provides a steady level of insulin over a 24-hour period. Examples include insulin glargine (Lantus), insulin detemir (Levemir), and insulin degludec (Tresiba).
In addition to insulin therapy, some people with type 1 diabetes may also take other medications to manage their blood sugar levels, such as
- Pramlintide (Symlin): This medication is used to help control blood sugar levels after meals. It is taken in addition to insulin therapy.
- Metformin: This medication is commonly used to treat type 2 diabetes, but it may also be used in some cases of type 1 diabetes to help control blood sugar levels.
- GLP-1 receptor agonists: These medications help to stimulate the production of insulin and lower blood sugar levels. They are usually used in combination with insulin therapy and are given by injection. Examples include exenatide (Byetta) and liraglutide (Victoza).
It is important to note that insulin therapy is the main treatment for type 1 diabetes, and medications such as metformin and GLP-1 receptor agonists are typically only used in combination with insulin therapy.
The specific medications and dosages used will vary depending on the individual’s needs and preferences, and should be determined in consultation with a healthcare professional.
Other medications also may be prescribed for people with type 1 diabetes, such as:
- High blood pressure medications: Your provider may prescribe angiotensin-converting enzyme (ACE) inhibitors or angiotensin II receptor blockers (ARBs) to help keep your kidneys healthy. These medications are recommended for people with diabetes who have blood pressures above 140/90 millimeters of mercury (mm Hg).
- Aspirin: Your provider may recommend you take baby or regular aspirin daily to protect your heart. Your provider may feel that you have an increased risk of a cardiovascular event. Your provider will discuss the risk of bleeding if you take aspirin.
- Cholesterol-lowering drugs: Cholesterol guidelines are stricter for people with diabetes because of their higher risk of heart disease.
The American Diabetes Association recommends that low-density lipoprotein (LDL, or “bad”) cholesterol be below 100 mg/dL (2.6 mmol/L). High-density lipoprotein (HDL, or “good”) cholesterol is recommended to be over 50 mg/dL (1.3 mmol/L) in women and over 40 mg/dL (1 mmol/L) in men. Triglycerides, another type of blood fat, should be less than 150 mg/dL (1.7 mmol/L).
Procedure for insulin intake:
The procedure for insulin intake may vary depending on the specific type of insulin being used and the individual’s healthcare provider’s recommendations. However, the general steps for insulin intake are as follows:

- Wash your hands thoroughly with soap and water.
- Check the insulin vial or pen to ensure that it is the correct type of insulin and has not expired.
- Prepare the injection site by cleaning it with an alcohol swab.
- Depending on the type of insulin being used, gently roll the insulin vial or pen between your palms to mix the insulin. Do not shake the vial or pen, as this can cause air bubbles to form.
- Draw up the correct dose of insulin into the syringe or pen, following the instructions provided by your healthcare provider.
- Pinch the skin at the injection site, and insert the needle at a 90-degree angle. For some types of insulin, your healthcare provider may recommend injecting at a different angle or into a different area of the body.
- Inject the insulin slowly and steadily.
- Remove the needle from the injection site, and apply gentle pressure with an alcohol swab if necessary.
- Dispose of the syringe or pen and any unused insulin according to your healthcare provider’s instructions.
- Record the time and dose of the insulin injection in a logbook or app to help track your blood sugar levels and insulin intake.
It is important to follow your healthcare provider’s instructions for insulin intake, including the recommended dose, injection site, and timing. In case of any difficulties, consultation with your health care provider is necessary
TYPE-2 DIABETES
What is Type 2 Diabetes ?
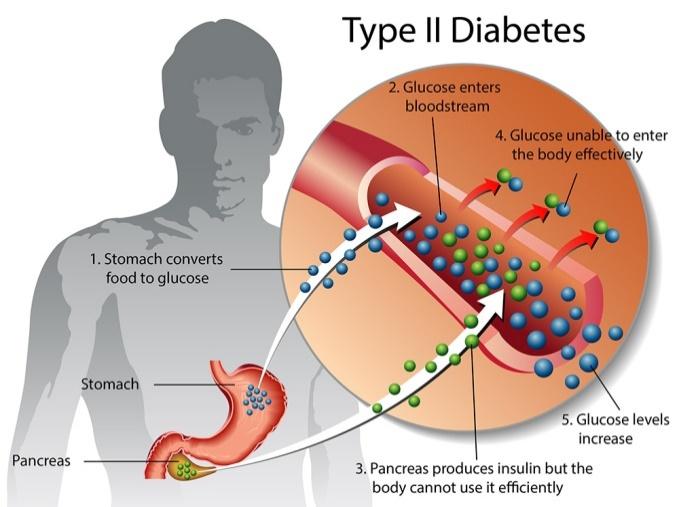
Type 2 diabetes is a chronic condition that affects how your body processes glucose, which is the main source of energy for your cells. In a healthy individual, the hormone insulin helps regulate the amount of glucose in the bloodstream by moving it into cells where it can be used for energy or stored for later use.
However, in people with type 2 diabetes, the body becomes resistant to insulin or doesn’t produce enough of it, which causes glucose to build up in the bloodstream. Over time, high levels of glucose in the blood can lead to a variety of complications, including damage to blood vessels, nerves, and organs.
Some of the risk factors for developing type 2 diabetes include being overweight or obese, having a family history of diabetes, being physically inactive, and having certain medical conditions like high blood pressure or high cholesterol.
Treatment for type 2 diabetes typically involves a combination of lifestyle changes and medication and may include monitoring blood sugar levels, managing weight through diet and exercise, and taking medications like insulin or oral diabetes medications. With proper management, many people with type 2 diabetes are able to live long, healthy lives.
Treatments
The treatment for type 2 diabetes typically involves a combination of lifestyle changes and medication. Some of the most common treatments for type-2 diabetes include
- Healthy diet
- Regular exercise
- Medication
- Blood sugar monitoring
- Weight Loss
- Managing other health conditions
Healthy diet: Eating a balanced and healthy diet that is low in sugar, fat, and salt can help manage blood sugar levels and promote weight loss.
Regular exercise: Regular physical activity can help improve insulin sensitivity, reduce blood sugar levels, and promote weight loss.
Medication: There are several types of medication that can be used to treat type 2 diabetes, including oral medications that help the body produce or use insulin more effectively, and injectable medications like insulin that help regulate blood sugar levels.
Blood sugar monitoring: Regular monitoring of blood sugar levels can help you and your doctor track how well your treatment plan is working and make adjustments as needed.
Weight loss: Losing weight through diet and exercise can help improve insulin sensitivity and reduce blood sugar levels.
Managing other health conditions: Managing other health conditions like high blood pressure and high cholesterol can help reduce the risk of complications from type 2 diabetes.
It’s important to work with your healthcare team to develop a treatment plan that works best for you, as the right treatment will depend on your individual needs and medical history. With proper management, many people with type 2 diabetes are able to live long, healthy lives.
Tests and Procedures used to diagnose type-2 diabetes include
There are several tests and procedures that can be used to diagnose type-2 diabetes. Some of the most common ones include
- Fasting plasma glucose (FPG) test: This test measures your blood sugar level after fasting for at least eight hours. A blood sugar level of 126 mg/dL (milligrams per deciliter) or higher is indicative of diabetes.
- Oral glucose tolerance test (OGTT): This test involves drinking a sugary solution and measuring your blood sugar level two hours later. A blood sugar level of 200 mg/dL or higher is indicative of diabetes.
- Hemoglobin A1C test: This test measures your average blood sugar level over the past two to three months. A hemoglobin A1C level of 6.5% or higher is indicative of diabetes.
- Random plasma glucose (RPG) test: This test measures your blood sugar level at a random time, regardless of when you last ate. A blood sugar level of 200 mg/dL or higher, accompanied by symptoms of diabetes, is indicative of diabetes.
- Urine test: This test checks for the presence of ketones in the urine, which can indicate uncontrolled diabetes.
Note:
If any of these tests indicate that you may have diabetes, your doctor may order additional tests to confirm the diagnosis and determine the type of diabetes you have. It’s important to note that early diagnosis and treatment of diabetes can help prevent or delay complications, so if you’re at risk for diabetes or have symptoms, talk to your doctor about getting tested.
Medication Drugs:
There are several types of medication drugs that can be used to treat type-2 diabetes. The choice of medication will depend on the individual’s specific needs and medical history. Some of the most common medication drugs for type 2 diabetes include:
- Metformin: This medication helps lower blood sugar levels by reducing the amount of glucose produced by the liver and increasing the body’s sensitivity to insulin.
- Sulfonylureas: These medications help stimulate the pancreas to produce more insulin.
- DPP-4 inhibitors: These medications help increase insulin production and decrease the amount of glucose produced by the liver.
- GLP-1 receptor agonists: These medications help increase insulin production and decrease the amount of glucose produced by the liver. They may also help reduce appetite and promote weight loss.
- SGLT2 inhibitors: These medications help lower blood sugar levels by increasing the amount of glucose excreted in the urine.
- Insulin: Injectable insulin may be needed if other medications are not able to control blood sugar levels effectively.
Note:
It’s important to work with your healthcare team to determine the best medication regimen for you, as the choice of medication will depend on several factors, including your medical history, lifestyle, and personal preferences. Additionally, it’s important to monitor blood sugar levels regularly when taking medication for type 2 diabetes.
Procedure for Metformin:
Metformin is a medication commonly used to treat type-2 diabetes. Here are some general guidelines for taking Metformin:

- Take it as directed: Follow your healthcare provider’s instructions for taking Metformin. It is typically taken once or twice a day with meals.
- Monitor blood sugar levels: Regularly monitoring your blood sugar levels can help you and your healthcare provider determine if your dose of Metformin needs to be adjusted.
- Be aware of potential side effects: Common side effects of Metformin include nausea, diarrhea, and stomach upset. These side effects usually improve over time, but if they persist, talk to your healthcare provider.
- Avoid excessive alcohol consumption: Drinking alcohol while taking Metformin can increase the risk of developing low blood sugar.
- Keep other healthcare providers informed: Let other healthcare providers, such as dentists or surgeons, know that you are taking Metformin, as it may interact with other medications.
- Do not skip doses: Taking Metformin consistently is important for maintaining stable blood sugar levels.
Note:
It’s important to work with your healthcare team to determine if Metformin is the right medication for you and to develop a treatment plan that is tailored to your individual needs and medical history. Additionally, it’s important to make lifestyle changes, such as eating a healthy diet and engaging in regular physical activity, to manage type 2 diabetes effectively.
Procedure for Sulfonylureas:
Sulfonylureas are a type of medication used to treat type-2 diabetes. Here are some general guidelines for taking Sulfonylureas:

- Take it as directed: Follow your healthcare provider’s instructions for taking Sulfonylureas. It is typically taken once or twice a day with meals.
- Monitor blood sugar levels: Regularly monitoring your blood sugar levels can help you and your healthcare provider determine if your dose of Sulfonylureas needs to be adjusted.
- Be aware of potential side effects: Common side effects of Sulfonylureas include low blood sugar, nausea, and weight gain. These side effects usually improve over time, but if they persist, talk to your healthcare provider.
- Be cautious with alcohol consumption: Drinking alcohol while taking Sulfonylureas can increase the risk of developing low blood sugar.
- Keep other healthcare providers informed: Let other healthcare providers, such as dentists or surgeons, know that you are taking Sulfonylureas, as it may interact with other medications.
- Do not skip doses: Taking Sulfonylureas consistently is important for maintaining stable blood sugar levels.
Note:
It’s important to work with your healthcare team to determine if Sulfonylureas is the right medication for you and to develop a treatment plan that is tailored to your individual needs and medical history. Additionally, it’s important to make lifestyle changes, such as eating a healthy diet and engaging in regular physical activity, to manage type 2 diabetes effectively.
Procedure for DPP-4
DPP-4 inhibitors are a type of medication used to treat type 2 diabetes. Here are some general guidelines for taking DPP-4 inhibitors:
- Take it as directed: Follow your healthcare provider’s instructions for taking DPP-4 inhibitors. It is typically taken once or twice a day with or without food.
- Monitor blood sugar levels: Regularly monitoring your blood sugar levels can help you and your healthcare provider determine if your dose of DPP-4 inhibitors needs to be adjusted.
- Be aware of potential side effects: Common side effects of DPP-4 inhibitors include headache, sore throat, and upper respiratory infections. These side effects usually improve over time, but if they persist, talk to your healthcare provider.
- Keep other healthcare providers informed: Let other healthcare providers, such as dentists or surgeons, know that you are taking DPP-4 inhibitors, as it may interact with other medications.
- Do not skip doses: Taking DPP-4 inhibitor consistently is important for maintaining stable blood sugar levels.
Note:
It’s important to work with your healthcare team to determine if DPP-4 inhibitors are the right medication for you and to develop a treatment plan that is tailored to your individual needs and medical history. Additionally, it’s important to make lifestyle changes, such as eating a healthy diet and engaging in regular physical activity, to manage type 2 diabetes effectively.
GESTATIONAL DIABETES
What is Gestational Diabetes ?
Gestational diabetes is a type of diabetes that develops during pregnancy. It occurs when the hormones produced by the placenta during pregnancy prevent insulin from functioning properly in the mother’s body, resulting in high blood sugar levels. Gestational diabetes can occur in any woman during pregnancy, but certain factors, such as obesity, a family history of diabetes, and advanced maternal age, increase the risk.
Gestational diabetes usually does not cause any symptoms, and it is usually detected through routine screening tests performed during pregnancy. If left untreated, gestational diabetes can lead to complications for both the mother and the baby, including preeclampsia, premature delivery, and macrosomia (a larger-than-average baby).
Managing gestational diabetes involves making lifestyle changes, such as following a healthy diet, exercising regularly, and monitoring blood sugar levels. In some cases, medication, such as insulin, may be necessary to control blood sugar levels. With proper management, most women with gestational diabetes are able to deliver healthy babies and return to normal blood sugar levels after pregnancy.

Treatments:
The treatment for gestational diabetes typically involves a combination of lifestyle changes and, in some cases, medication. The goal of treatment is to keep blood sugar levels within a target range to prevent complications for both the mother and the baby.
- Diet and exercise: Women with gestational diabetes are advised to follow a healthy eating plan that includes whole grains, fruits, vegetables, lean protein, and low-fat dairy products. They are also encouraged to engage in moderate physical activity, such as walking or swimming, for at least 30 minutes a day.
- Blood sugar monitoring: Women with gestational diabetes are advised to monitor their blood sugar levels regularly, usually several times a day, to ensure they are within the target range. This can be done with a glucose meter or a continuous glucose monitor.
- Medication: In some cases, medication, such as insulin or an oral medication called glyburide, may be necessary to help manage blood sugar levels. Insulin is the preferred medication during pregnancy because it does not cross the placenta, while other medications may have potential risks to the developing fetus.
- Fetal monitoring: Women with gestational diabetes may also need to have regular ultrasounds to monitor fetal growth and ensure the baby is not too large, which could increase the risk of complications during delivery.
- Delivery: The timing and mode of delivery will depend on a variety of factors, including blood sugar control, fetal growth, and maternal health. In some cases, early delivery or a cesarean section may be recommended.
Note:
It is important for women with gestational diabetes to work closely with their healthcare providers to develop an individualized treatment plan that is safe and effective for both the mother and the baby.
Tests and Procedures used to diagnose Gestational Diabetes include:
There are several tests and procedures used to diagnose gestational diabetes:
- Glucose Challenge Test (GCT): This is a screening test that is usually done between 24 and 28 weeks of pregnancy. The woman drinks a sugary drink and her blood sugar is tested after one hour. If the blood sugar level is high, further testing is done.
- Oral Glucose Tolerance Test (OGTT): If the GCT result is abnormal, an OGTT is done. The woman fasts overnight, then drink a sugary drink and has her blood sugar levels tested at fasting, 1 hour, 2 hours, and 3 hours after drinking the solution.
- Hemoglobin A1c (HbA1c): This test measures the average blood sugar levels over the past 2-3 months. It is not typically used to diagnose gestational diabetes but may be used in some cases.
- Continuous Glucose Monitoring (CGM): This is a device that is worn by the woman to monitor her blood sugar levels continuously. It is typically used in women with pre-existing diabetes but may be used in some cases of gestational diabetes.
If gestational diabetes is diagnosed, additional tests may be done to monitor the health of the mother and the baby, including fetal ultrasound to monitor fetal growth, and non-stress testing to monitor fetal well-being.
It is important for women to attend all recommended prenatal appointments and undergo appropriate testing to diagnose and manage gestational diabetes to ensure the best possible outcomes for both the mother and the baby.
Medication drugs:
The first-line treatment for gestational diabetes typically involves lifestyle changes, such as a healthy diet and regular exercise. However, in some cases, medication may be necessary to help manage blood sugar levels. The most commonly used medication for gestational diabetes is insulin, but there are other options available as well, including
- Insulin: Insulin is a hormone that helps the body use glucose for energy. It is typically injected under the skin using a syringe or an insulin pen. Insulin is safe to use during pregnancy because it does not cross the placenta, and it is the preferred medication for women with gestational diabetes who require medication to manage their blood sugar levels.
- Glyburide: Glyburide is an oral medication that is sometimes used to treat gestational diabetes. It works by increasing the body’s production of insulin. However, there is some concern about the safety of glyburide during pregnancy, and insulin is generally considered the first-line treatment.
- Metformin: Metformin is another oral medication that is sometimes used to treat gestational diabetes. It works by reducing the amount of glucose produced by the liver and improving insulin sensitivity. However, there is limited data on the safety of metformin during pregnancy, and it is not as effective as insulin at controlling blood sugar levels.
It is important for women with gestational diabetes to work closely with their healthcare providers to determine the best course of treatment for their individual situation. This may involve a combination of lifestyle changes and medication to manage blood sugar levels and ensure the best possible outcomes for both the mother and the baby.
Procedure for Insulin:
The procedure for administering insulin to treat gestational diabetes may vary depending on the specific type of insulin being used and the individual woman’s needs. However, the general steps for administering insulin are as follows:

- Wash your hands thoroughly with soap and water.
- Check the insulin label to make sure it is the correct type and has not expired.
- Roll the insulin bottle between your palms to mix the insulin. Do not shake the bottle, as this can cause bubbles to form, which can affect the accuracy of the dose.
- Clean the injection site with an alcohol swab and allow the skin to dry.
- Pinch a fold of skin at the injection site to create a small “tent”.
- Hold the syringe like a pencil and insert the needle into the skin at a 90-degree angle. Make sure the needle goes all the way into the skin.
- Push the plunger down slowly and steadily to inject the insulin.
- Count to 5 before removing the needle to ensure that all the insulin has been injected.
- Release the skin fold and remove the needle from the skin.
- Discard the needle and syringe in a puncture-proof container.
- Record the date, time, and dose of insulin in a logbook or on a smartphone app.
Note:
It is important to follow your healthcare provider’s instructions for administering insulin and to attend all recommended appointments to monitor blood sugar levels and ensure the best possible outcomes for both the mother and the baby.
Procedure for Glyburide:
The procedure for administering glyburide to treat gestational diabetes may vary depending on the specific dosage and frequency prescribed by the healthcare provider. However, the general steps for administering glyburide are as follows:
- Wash your hands thoroughly with soap and water.
- Check the glyburide label to make sure it is the correct medication and has not expired.
- Take the glyburide tablet with a glass of water or as directed by your healthcare provider. It is usually taken once or twice a day with a meal.
- Follow your healthcare provider’s instructions for monitoring your blood sugar levels to ensure that the glyburide is working effectively.
- Record the date, time, and dose of glyburide in a logbook or on a smartphone app.
Note:
It is important to follow your healthcare provider’s instructions for administering glyburide and to attend all recommended appointments to monitor blood sugar levels and ensure the best possible outcomes for both the mother and the baby. It is also important to be aware of the potential side effects of glyburide, including low blood sugar levels (hypoglycemia) and other adverse reactions, and to contact your healthcare provider if you experience any symptoms or have concerns about the medication.
Procedure for Metformin:
The procedure for administering metformin to treat gestational diabetes may vary depending on the specific dosage and frequency prescribed by the healthcare provider. However, the general steps for administering metformin are as follows:

- Wash your hands thoroughly with soap and water.
- Check the metformin label to make sure it is the correct medication and has not expired.
- Take the metformin tablet with a glass of water or as directed by your healthcare provider. It is usually taken once or twice a day with a meal.
- Follow your healthcare provider’s instructions for monitoring your blood sugar levels to ensure that the metformin is working effectively.
- Record the date, time, and dose of metformin in a logbook or on a smartphone app.
Note:
It is important to follow your healthcare provider’s instructions for administering metformin and to attend all recommended appointments to monitor blood sugar levels and ensure the best possible outcomes for both the mother and the baby. It is also important to be aware of the potential side effects of metformin, including gastrointestinal symptoms such as nausea, vomiting, and diarrhea, and to contact your healthcare provider if you experience any symptoms or have concerns about the medication.




