Heart Disease
Heart disease, also known as cardiovascular disease, refers to a group of conditions that affect the heart and blood vessels. These conditions can include coronary artery disease, heart failure, arrhythmias, and valve disorders, among others. Heart disease is a leading cause of death worldwide, and risk factors for developing it include high blood pressure, high cholesterol, smoking, diabetes, family history, and obesity. Symptoms of heart disease can vary depending on the specific condition but can include chest pain or discomfort, shortness of breath, fatigue, and palpitations. Early diagnosis and management of heart disease can help prevent complications and improve outcomes. Treatment options can include lifestyle modifications, medication, and in some cases, surgery.
Types of Heart Diseases
- Coronary artery disease (CAD): This is the most common type of heart disease, and it is caused by the buildup of plaque in the arteries that supply blood to the heart.
- Heart failure: This occurs when the heart is unable to pump blood effectively, leading to fatigue, shortness of breath, and other symptoms.
- Arrhythmias: These are irregular heart rhythms that can be caused by various factors, including heart disease, stress, and certain medications.
- Atherosclerosis: This is a condition in which the arteries become narrowed or blocked due to a buildup of fatty deposits.
- Heart valve disease: This occurs when one or more of the heart’s valves don’t work properly, leading to symptoms such as chest pain, shortness of breath, and fatigue.
- Cardiomyopathy: This is a condition in which the heart muscle becomes weakened or enlarged, leading to a range of symptoms, including fatigue, shortness of breath, and chest pain.
- Congenital heart disease: This is a type of heart disease that is present at birth, and it can involve a range of structural abnormalities in the heart.
- Myocarditis: This is an inflammation of the heart muscle that can be caused by a viral infection, certain medications, or other factors.
- Hypertensive heart disease: This occurs when high blood pressure causes damage to the heart and its blood vessels over time.
- Peripheral artery disease: This is a type of heart disease that affects the arteries outside of the heart, most commonly in the legs, and it can cause symptoms such as pain, numbness, and weakness.
CORONARY ARTERY DISEASE (CAD)

Coronary artery disease (CAD) is a common type of heart disease that occurs when the arteries that supply blood to the heart become narrow or blocked. This narrowing or blockage is typically caused by the build-up of fatty deposits, called plaque, inside the arteries.
CAD can lead to a range of symptoms, including chest pain or discomfort (angina), shortness of breath, fatigue, and weakness. In some cases, CAD can also cause a heart attack, which occurs when the blood flow to a part of the heart is blocked, leading to damage or death of the heart muscle.
Risk factors for CAD include high blood pressure, high cholesterol, smoking, obesity, diabetes, and a family history of heart disease. Lifestyle changes, such as a healthy diet, regular exercise, and avoiding smoking, can help reduce the risk of CAD. In addition, medications such as statins, blood pressure-lowering drugs, and antiplatelet agents can be used to manage CAD and reduce the risk of heart attack.
Treatment for CAD may also include procedures such as angioplasty, in which a balloon is used to open a blocked artery, or coronary artery bypass grafting (CABG), in which a blood vessel from elsewhere in the body is used to bypass a blocked artery. In severe cases, heart transplantation may be necessary.
Treatments
The treatment of coronary artery disease (CAD) depends on the severity of the disease, the presence of symptoms, and other factors such as age, overall health, and medical history. Here are some common treatments for CAD:
- Lifestyle changes: Making healthy lifestyle changes, such as quitting smoking, adopting a healthy diet, losing weight, and getting regular exercise, can help reduce the risk of CAD and manage the disease.
- Medications: Medications such as statins, aspirin, beta-blockers, calcium channel blockers, and nitro-glycerine may be prescribed to lower cholesterol, reduce blood pressure, prevent blood clots, and manage symptoms such as chest pain.
- Angioplasty and stenting: This is a minimally invasive procedure in which a balloon is used to open a blocked or narrowed artery, and a stent is placed to keep the artery open.
- Coronary artery bypass grafting (CABG): In this surgery, a blood vessel from another part of the body is used to bypass the blocked or narrowed artery, restoring blood flow to the heart.
- Trans myocardial laser revascularization (TMR): This is a procedure in which a laser is used to create tiny channels in the heart muscle to improve blood flow.
- Enhanced external counter pulsation (EECP): This is a non-invasive treatment that involves wearing inflatable cuffs on the legs that are timed to inflate and deflate with the heartbeat, improving blood flow to the heart.
- Heart transplant: In severe cases, a heart transplant may be necessary to replace a damaged or diseased heart with a healthy one.
The treatment plan for CAD is individualized and will depend on the severity of the disease and the patient’s overall health. A doctor can help determine the best treatment approach based on the patient’s specific needs.
Tests and Procedures to diagnose Coronary Artery Disease (CAD):
There are several tests and procedures that can be used to diagnose coronary artery disease (CAD) and evaluate the severity of the disease. Here are some common tests and procedures:
- Electrocardiogram (ECG): An ECG is a test that records the electrical activity of the heart and can help detect abnormalities in heart rhythm or blood flow.
- Stress test: A stress test is a type of ECG that is performed while the patient is exercising or under stress, such as with medication, to evaluate the heart’s response to increased activity.
- Echocardiogram: An echocardiogram is a non-invasive test that uses ultrasound to create images of the heart and evaluate its function and blood flow.
- Cardiac catheterization: This is an invasive procedure in which a thin, flexible tube called a catheter is inserted into a blood vessel and guided to the heart. Contrast dye is injected to make the arteries visible on X-ray, and measurements of pressure and blood flow can be taken.
- Coronary angiography: This is a type of cardiac catheterization that involves injecting contrast dye into the coronary arteries to evaluate the degree of narrowing or blockage.
- CT angiography: This is a non-invasive imaging test that uses X-rays and a contrast dye to create detailed images of the coronary arteries and identify areas of blockage.
- Magnetic resonance imaging (MRI): This is a non-invasive imaging test that uses a magnetic field and radio waves to create detailed images of the heart and blood vessels.
- PET scan: This is an imaging test that uses a small amount of radioactive tracer to evaluate blood flow and metabolism in the heart.
A doctor may recommend one or more of these tests or procedures based on the patient’s symptoms, medical history, and other factors. These tests can help diagnose CAD and guide treatment decisions.
Procedure for Angioplasty and stenting in Coronary Artery Disease
Angioplasty and stenting are two common procedures used to treat coronary artery disease (CAD) by opening blocked or narrowed coronary arteries. Here’s an overview of the procedure:
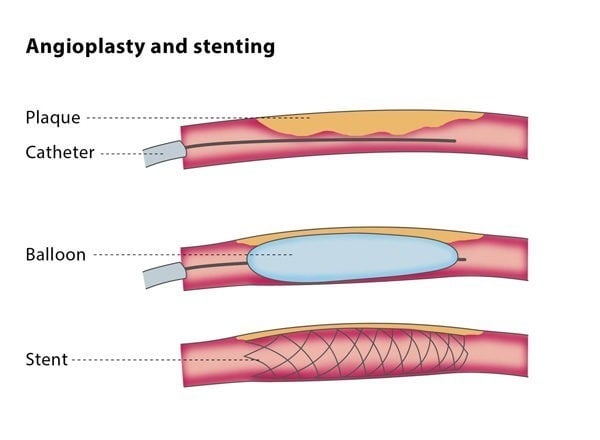
- Preparation: The patient is given medication to help them relax and a local anesthetic is applied to numb the area where the catheter will be inserted, usually in the groin or wrist.
- Catheter insertion: A thin, flexible tube called a catheter is inserted into the blood vessel and guided to the blocked or narrowed coronary artery using X-ray guidance.
- Balloon inflation: A small balloon at the tip of the catheter is inflated to widen the narrowed section of the artery and improve blood flow.
- Stent placement: After the balloon is inflated, a small metal mesh tube called a stent may be inserted into the artery to help keep it open. The stent remains in place permanently.
- Removal: The catheter is removed and pressure is applied to the insertion site to prevent bleeding.
The procedure typically takes about 30-60 minutes and is performed under local anesthesia, meaning the patient is awake but may be sedated. Most patients can go home the same day or the following day.
Angioplasty and stenting can be effective in improving blood flow to the heart and reducing symptoms such as chest pain. However, like any procedure, there are risks, including bleeding, infection, and blood clots. The doctor will discuss the risks and benefits of the procedure with the patient before it is performed.
Procedure for Coronary artery bypass grafting (CABG)
Coronary artery bypass grafting (CABG) is a surgical procedure used to treat severe coronary artery disease (CAD) by creating a new route for blood to flow around blocked or narrowed arteries. Here’s an overview of the procedure:
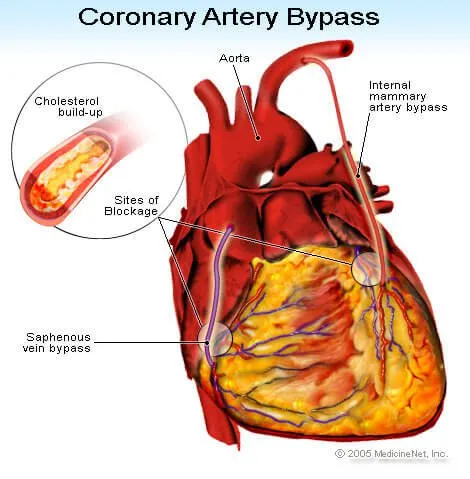
- Anesthesia: The patient is given general anesthesia, meaning they are asleep and feel no pain during the procedure.
- Incision: A large incision is made in the chest to access the heart and coronary arteries.
- Harvesting the graft: A healthy blood vessel is removed from another part of the body, such as the leg, to use as a graft. This vessel is usually the saphenous vein or the internal mammary artery.
- Connecting the graft: The graft is then attached to the blocked or narrowed coronary artery, creating a new route for blood to flow around the blockage.
- Completion: After all grafts have been completed, the heart is restarted and blood flow is restored. The chest incision is then closed with stitches or staples.
The procedure can take several hours and may require a hospital stay of several days to a week. Patients will need to rest and limit physical activity for several weeks after the procedure to allow the chest incision to heal.
CABG can be an effective treatment for severe CAD, particularly in cases where multiple arteries are blocked or the left main coronary artery is affected. However, like any surgery, there are risks, including bleeding, infection, and complications related to anesthesia. The doctor will discuss the risks and benefits of the procedure with the patient before it is performed.
Procedure for Trans myocardial laser revascularization (TMR)
Trans myocardial laser revascularization (TMR) is a surgical procedure used to treat severe angina, a type of chest pain caused by reduced blood flow to the heart, in patients who are not candidates for traditional coronary artery bypass surgery. Here’s an overview of the procedure:

- Anesthesia: The patient is given general anesthesia, meaning they are asleep and feel no pain during the procedure.
- Incision: A small incision is made in the chest to access the heart.
- Laser therapy: A high-energy laser is used to create channels, or “microscopic holes,” in the heart muscle. This is intended to improve blood flow by allowing oxygenated blood from the heart’s chambers to enter the oxygen-deprived heart muscle directly.
- Completion: After the laser therapy is complete, the incision is closed with stitches or staples.
The procedure typically takes several hours and may require a hospital stay of several days to a week. Patients will need to rest and limit physical activity for several weeks after the procedure to allow the chest incision to heal.
TMR can be an effective treatment for severe angina in patients who are not candidates for traditional bypass surgery or angioplasty. However, like any surgery, there are risks, including bleeding, infection, and complications related to anesthesia. The effectiveness of TMR is also somewhat controversial, and it is generally considered a last-resort treatment option. The doctor will discuss the risks and benefits of the procedure with the patient before it is performed.
HEART FAILURE
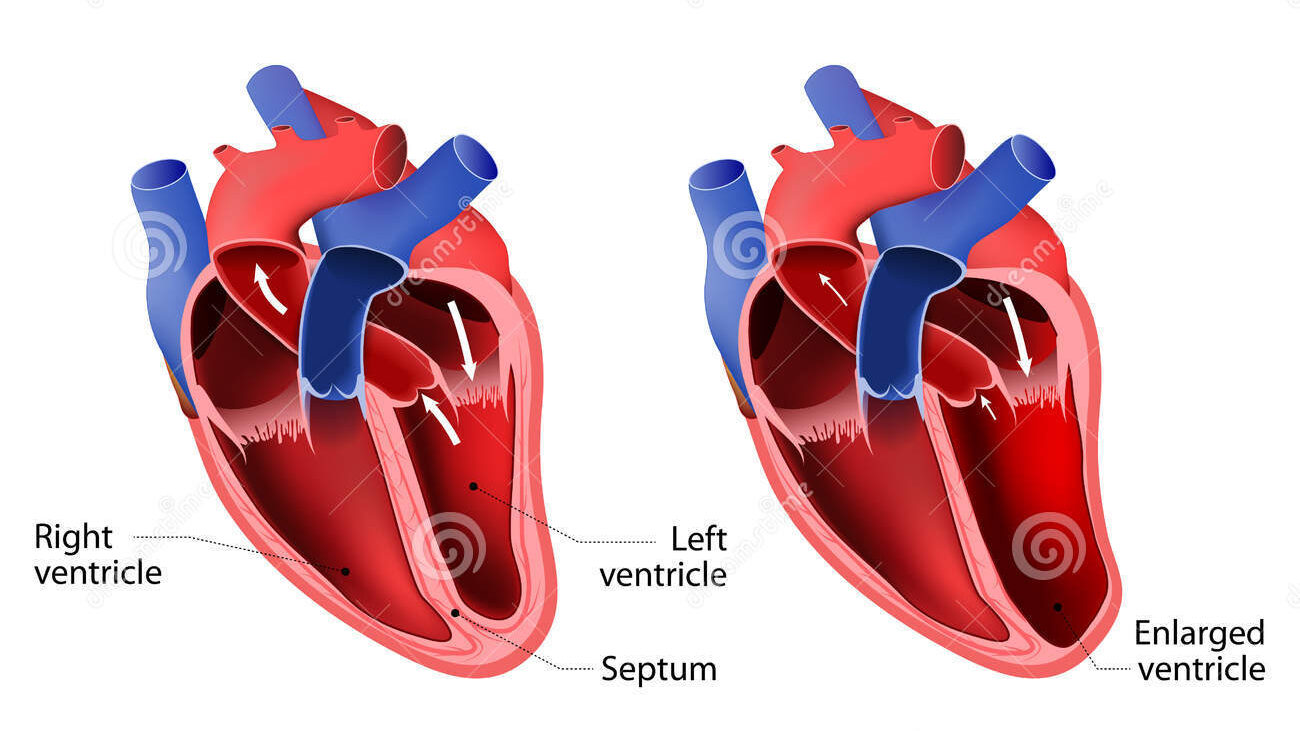
Heart failure is a chronic condition in which the heart is unable to pump enough blood to meet the body’s needs. It can develop gradually over time or occur suddenly as a result of a heart attack or other cardiovascular event. Heart failure can affect either the left side, right side, or both sides of the heart, and can lead to a range of symptoms and complications.
Symptoms of heart failure can include:
- Shortness of breath, especially during physical activity or while lying down
- Fatigue or weakness
- Swelling in the legs, ankles, or feet
- Rapid or irregular heartbeat
- Persistent cough or wheezing
- Reduced ability to exercise or perform physical activity
There are many different causes of heart failure, including coronary artery disease, high blood pressure, diabetes, and other cardiovascular conditions. Treatment for heart failure typically focuses on managing symptoms, improving heart function, and preventing complications. This may involve medications, lifestyle changes such as a heart-healthy diet and regular exercise, and, in severe cases, surgical interventions such as heart transplantation.
The prognosis for heart failure varies depending on the severity of the condition and the underlying causes. With proper management, many people with heart failure are able to live active and fulfilling lives, but in some cases, the condition can be life-threatening. Regular monitoring and ongoing care are important for people with heart failure to help manage their symptoms and prevent complications.
Treatments
Treatment for heart failure typically involves a combination of medications, lifestyle changes, and, in some cases, surgical interventions. The goal of treatment is to improve heart function, manage symptoms, and prevent complications. Here are some of the main treatments for heart failure:
Medications: There are several different types of medications used to treat heart failure, including:
- ACE inhibitors and ARBs: These medications help to relax blood vessels and improve blood flow.
- Beta blockers: These medications slow the heart rate and reduce the workload on the heart.
- Diuretics: These medications help to remove excess fluid from the body, reducing swelling and improving breathing.
- Aldosterone antagonists: These medications help to reduce fluid buildup and improve heart function.
- Digoxin: This medication helps to improve heart function and regulate the heart rate.
Lifestyle changes: Making lifestyle changes can help to improve heart function and manage symptoms of heart failure. These may include:
- Following a heart-healthy diet low in sodium and saturated fat.
- Maintaining a healthy weight.
- Regular exercise, as recommended by a healthcare provider.
- Quitting smoking and avoiding alcohol.
- Managing stress.
Surgical interventions: In some cases, surgical interventions may be needed to treat heart failure. These may include:
- Implantable devices such as pacemakers or defibrillators, which can help to regulate heart rhythm.
- Coronary artery bypass surgery or angioplasty, which can improve blood flow to the heart.
- Heart transplant, in cases of severe heart failure that cannot be managed with other treatments.
Treatment for heart failure is typically ongoing and may involve regular monitoring and adjustments to m
Tests and Procedure to diagnose Heart Failure:
There are several tests and procedures that may be used to diagnose heart failure. Here are some of the most common:
- Physical exam: The doctor will listen to the patient’s heart and lungs, check for signs of fluid buildup (edema) in the legs and ankles, and assess the patient’s overall health.
- Echocardiogram: This is a non-invasive test that uses sound waves to create images of the heart. It can show the size and shape of the heart, how well the heart is pumping, and whether there are any abnormalities in the heart valves or chambers.
- Electrocardiogram (ECG): This test measures the electrical activity of the heart and can help identify abnormal heart rhythms or damage to the heart muscle.
- Chest X-ray: This can show whether the heart is enlarged or whether there is fluid buildup in the lungs.
- Blood tests: These can check for certain markers that may indicate heart failure, such as elevated levels of B-type natriuretic peptide (BNP) or troponin.
- Cardiac catheterization: This involves inserting a thin, flexible tube (catheter) into a blood vessel in the groin or arm and threading it up to the heart. This can help the doctor measure pressures inside the heart, take pictures of the arteries, and check for blockages.
- Stress test: This test involves exercising on a treadmill or stationary bike while the doctor monitors the heart’s response. It can help identify whether there is reduced blood flow to the heart during exertion.
- MRI or CT scan: These imaging tests can provide detailed images of the heart and can help diagnose heart failure, assess heart function, and check for other conditions that may be contributing to symptoms.
Medications
There are several different types of medications used to treat heart failure. These medications work in different ways to help improve heart function, manage symptoms, and prevent complications. Here are some of the most commonly used medications for heart failure:
- ACE inhibitors: ACE inhibitors help to relax blood vessels and improve blood flow, reducing the workload on the heart. Examples include enalapril, lisinopril, and ramipril.
- ARBs: ARBs are similar to ACE inhibitors in that they help to relax blood vessels and improve blood flow. They are often used as an alternative to ACE inhibitors in people who cannot tolerate them. Examples include losartan, valsartan, and candesartan.
- Beta blockers: Beta blockers help to slow the heart rate and reduce the workload on the heart. They can also help to improve heart function over time. Examples include carvedilol, metoprolol, and bisoprolol.
- Diuretics: Diuretics help to remove excess fluid from the body, reducing swelling and improving breathing. They are often used to manage symptoms such as shortness of breath and fluid build-up in the lungs or legs. Examples include furosemide, hydrochlorothiazide, and spironolactone.
- Aldosterone antagonists: Aldosterone antagonists help to reduce fluid build-up and improve heart function. They are often used in combination with other medications to manage heart failure. Examples include spironolactone and eplerenone.
- Digoxin: Digoxin helps to improve heart function and regulate the heart rate. It is often used in combination with other medications to manage heart failure.
It is important to note that medication regimens for heart failure are often complex and may involve multiple medications taken at different times of day. It is important to follow a healthcare provider’s instructions carefully and to report any side effects or changes in symptoms promptly. Medication or lifestyle changes as needed. The goal is to help people with heart failure manage their symptoms, improve their quality of life, and reduce the risk of complications.
Procedure for Angioplasty:
The procedure for angioplasty for coronary artery disease is similar to the general angioplasty procedure, but with some additional steps:

- Preparation: The patient is given a sedative to help them relax and a local anesthetic is used to numb the area where the catheter will be inserted.
- Insertion of catheter: A thin, flexible tube called a catheter is inserted into an artery in the groin or arm and threaded through the blood vessels to the blocked or narrowed coronary artery.
- Angiogram: Once the catheter is in place, a contrast dye is injected through the catheter and X-ray images are taken to visualize the inside of the coronary arteries.
- Guidewire and balloon catheter: A guidewire is then inserted through the catheter and advanced to the site of the blockage. A balloon catheter is then threaded over the guidewire and positioned at the site of the blockage.
- Inflation of balloon: The balloon is inflated, which compresses the plaque or fatty deposits against the walls of the artery and opens up the blockage, allowing for improved blood flow.
- Stent placement: In most cases, a stent (a small metal mesh tube) is then inserted at the site of the blockage to help keep the artery open and prevent it from closing again. The stent is collapsed around the balloon catheter, and when the balloon is inflated, the stent expands and is left in place.
- Angiogram and removal of catheter: After the stent is in place, another angiogram is performed to ensure that the artery is open and blood flow is restored. The catheter and guidewire are then removed and pressure is applied to the puncture site to prevent bleeding.
The patient may need to stay in the hospital for a day or two after the procedure for monitoring and recovery. In some cases, medication may be prescribed to help prevent blood clots and other complications.
Procedure for Heart Transplant
A heart transplant is a surgical procedure that involves replacing a diseased or damaged heart with a healthy heart from a donor. Here are the general steps involved in a heart transplant.

- Evaluation and preparation: The patient is evaluated to determine if they are a good candidate for a heart transplant. This includes a medical history review, physical examination, lab tests, and imaging studies. The patient may need to make lifestyle changes and undergo treatments to prepare for the surgery.
- Placement on the transplant waiting list: If the patient is determined to be a good candidate, they are placed on the national transplant waiting list. The wait time for a heart transplant can vary, depending on factors such as the patient’s blood type, medical urgency, and availability of donor organs.
- Donor heart procurement: When a donor heart becomes available, the transplant team is notified and the donor heart is procured. The donor heart is carefully screened for compatibility and the absence of disease.
- Surgery: The patient is brought to the operating room and placed under general anesthesia. A large incision is made in the chest, and the diseased heart is removed. The donor heart is then carefully placed in the patient’s chest and connected to the blood vessels and other structures in the chest. The surgery can take several hours to complete.
- Recovery: After the surgery, the patient is closely monitored in the intensive care unit for several days. They will be given medications to prevent rejection of the donor heart and to manage pain and other symptoms. Physical therapy and other rehabilitation may be necessary to help the patient regain strength and function.
- Follow-up care: The patient will need ongoing follow-up care with the transplant team to monitor the function of the donor heart, manage medications, and address any complications or issues that arise. They will need to make lifestyle changes and take medications for the rest of their life to prevent rejection and ensure the long-term success of the transplant.
ARRHYTHMIAS
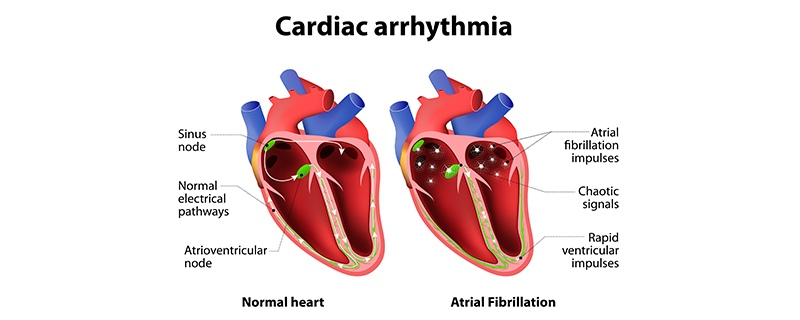
Arrhythmias refer to abnormal heart rhythms or irregular heartbeats. The heart normally beats in a regular, coordinated rhythm, but with arrhythmias, the heart may beat too fast, too slow, or irregularly. Arrhythmias can occur in the upper chambers of the heart (atria) or the lower chambers of the heart (ventricles).
Arrhythmias can occur for many reasons, including underlying heart disease, genetic factors, medication side effects, and electrolyte imbalances. Symptoms of arrhythmias may include palpitations, light headedness, dizziness, fainting, chest pain, or shortness of breath. Treatment for arrhythmias may involve medication, lifestyle changes, implantable devices (such as pacemakers or defibrillators), or procedures such as catheter ablation or cardioversion.
Treatments:
The treatment for arrhythmias depends on the type and severity of the arrhythmia, as well as the individual’s overall health. Here are some common treatments for arrhythmias.
- Medications: There are several medications that can be used to treat arrhythmias, such as beta-blockers, calcium channel blockers, and anti-arrhythmic drugs. These medications work by slowing down the heart rate, regulating the heartbeat, or preventing abnormal heart rhythms.
- Cardioversion: This is a procedure in which a controlled electric shock is delivered to the heart to restore a normal heart rhythm. There are two types of cardioversion: electrical cardioversion (using an electrical shock) and chemical cardioversion (using medication).
- Catheter ablation: This is a minimally invasive procedure that involves using radiofrequency energy or freezing to destroy small areas of heart tissue that may be causing the arrhythmia.
- Pacemaker: A pacemaker is a small device that is implanted under the skin and connected to the heart to regulate the heartbeat. It sends electrical signals to the heart to keep it beating at a steady rate.
- Implantable cardioverter-defibrillator (ICD): An ICD is a device that is implanted under the skin and connected to the heart. It monitors the heart rhythm and delivers a shock to the heart if it detects a dangerous arrhythmia.
- Surgery: In some cases, surgery may be necessary to treat arrhythmias, such as the Maze procedure, which involves creating scar tissue in the heart to prevent abnormal electrical signals from causing arrhythmias.
- Lifestyle changes: Making healthy lifestyle changes such as quitting smoking, losing weight, reducing stress, and limiting alcohol and caffeine intake can help reduce the frequency and severity of some types of arrhythmias.
Tests and Procedures to diagnose Arrhythmias
There are several tests and procedures that can be used to diagnose arrhythmias. Here are some of the most common.
- Electrocardiogram (ECG or EKG): This is a simple, non-invasive test that records the electrical activity of the heart. It involves placing electrodes on the chest, arms, and legs, and takes only a few minutes to complete.
- Holter monitor: This is a portable device that records the heart’s electrical activity over a period of 24 to 48 hours. It allows doctors to detect any arrhythmias that may occur during normal daily activities.
- Event recorder: This is a small device that is worn for several weeks and can be activated by the patient when they feel symptoms of an arrhythmia. It records the heart’s electrical activity during the event, which can help diagnose the type of arrhythmia.
- Echocardiogram: This is a non-invasive test that uses sound waves to create images of the heart. It can help diagnose structural abnormalities or heart disease that may be causing arrhythmias.
- Electrophysiology study (EPS): This is an invasive procedure that involves inserting catheters into the heart to record its electrical activity. It can help identify the location and cause of an arrhythmia, and may be used to guide treatment options such as catheter ablation.
- Tilt table test: This test involves tilting a patient from a lying to a standing position while monitoring their heart rate and blood pressure. It can help diagnose certain types of arrhythmias, such as vasovagal syncope.
- Genetic testing: In some cases, genetic testing may be used to identify genetic mutations that may cause arrhythmias such as long QT syndrome.
Overall, a combination of these tests and procedures may be used to diagnose arrhythmias and determine the most appropriate treatment plan.
Medications
There are several medications that can be used to treat arrhythmias, depending on the type and severity of the arrhythmia. Here are some common medications for arrhythmias:
- Anti-arrhythmic drugs: These medications work by controlling the electrical signals in the heart to prevent abnormal heart rhythms. Examples include amiodarone, flecainide, and propafenone.
- Beta-blockers: These medications block the effects of adrenaline on the heart, slowing down the heart rate and reducing the workload of the heart. Examples include metoprolol, propranolol, and atenolol.
- Calcium channel blockers: These medications work by blocking calcium from entering the heart muscle cells, which can slow down the heart rate and reduce the strength of the heart’s contractions. Examples include verapamil and diltiazem.
- Blood thinners: These medications, also known as anticoagulants, can help reduce the risk of blood clots forming in the heart and causing a stroke. Examples include warfarin, apixaban, and dabigatran.
- Digitalis: This medication works by increasing the strength of the heart’s contractions, which can be helpful for some types of arrhythmias, such as atrial fibrillation. It is derived from the foxglove plant.
It’s important to note that all medications have potential side effects and can interact with other medications, so it’s important to work closely with a healthcare provider to determine the most appropriate medication and dosage for your individual needs.
Procedure for Cardioversion
Cardioversion is a medical procedure that is used to restore the heart’s normal rhythm in patients with certain types of arrhythmias, such as atrial fibrillation or ventricular tachycardia. Here are the general steps of a cardioversion procedure:

- Preparation: The patient will be given instructions to follow before the procedure, such as avoiding food and drink for a certain amount of time. An IV line will also be inserted into the patient’s arm to deliver medication or sedation, if needed.
- Electrodes placement: Electrodes will be placed on the patient’s chest to monitor the heart’s electrical activity and deliver the electrical shock to the heart if necessary.
- Sedation or anesthesia: Depending on the patient’s needs and the type of cardioversion, the patient may be given medication to relax or be put under general anesthesia.
- Shock delivery: When the patient is sedated, the healthcare provider will deliver a controlled electrical shock to the heart through the electrodes on the chest. This shock can “reset” the heart’s rhythm to normal.
- Monitoring: After the shock is delivered, the healthcare provider will monitor the patient’s heart rhythm and blood pressure to ensure that the procedure was successful and that the patient is stable.
- Recovery: The patient will be monitored for a period of time after the procedure to ensure there are no complications. They may be given medication to manage any pain or discomfort and will be given instructions to follow for their recovery, such as avoiding heavy lifting or strenuous activity for a certain amount of time.
It’s important to note that cardioversion may not be effective for all types of arrhythmias, and that the risks and benefits of the procedure will be discussed with the patient before it is performed.
Procedure for Catheter ablation
Catheter ablation is a medical procedure used to treat certain types of abnormal heart rhythms or arrhythmias. The procedure involves using a thin, flexible tube called a catheter, which is guided through a vein or artery and into the heart. Once inside the heart, the catheter delivers energy to the specific areas that are causing the abnormal heart rhythm, thereby destroying the tissue causing the arrhythmia.
Here is a general overview of the steps involved in a catheter ablation procedure:
- Preparation: Before the procedure, the patient is given anesthesia or sedation to help them relax and reduce any pain or discomfort. The patient’s vital signs are monitored, and any necessary medical equipment is attached, such as an ECG machine.
- Accessing the heart: The catheter is inserted into a blood vessel in the groin, neck, or arm and guided through the blood vessels into the heart. X-ray or ultrasound imaging is used to guide the catheter to the appropriate location within the heart.
- Mapping the heart: Once the catheter is inside the heart, it is used to map the electrical activity of the heart and identify the specific areas that are causing the abnormal heart rhythm.
- Ablation: Once the problem area has been identified, the catheter is used to deliver energy, such as radiofrequency or cryotherapy, to the specific location in the heart tissue. The energy destroys the tissue causing the arrhythmia, which helps restore a normal heart rhythm.
- Monitoring: During and after the procedure, the patient’s heart rate and rhythm are closely monitored to ensure that the ablation was successful and that the patient is stable.
- Recovery: After the procedure, the patient will need to stay in the hospital for a short time to recover. The catheter insertion site may be covered with a bandage or dressing, and the patient may need to lie flat for a few hours to prevent bleeding. The patient may need to avoid certain activities, such as lifting heavy objects, for a short time after the procedure.
Overall, the catheter ablation procedure is a minimally invasive treatment that can be highly effective in treating certain types of heart arrhythmias. The procedure can take a few hours, and the patient can usually return home on the same day or the next day after the procedure.
Procedure for Implantable cardioverter-defibrillator (ICD):
An Implantable cardioverter-defibrillator (ICD) is a medical device that is implanted under the skin in the chest to monitor and treat life-threatening arrhythmias or irregular heartbeats. The ICD device constantly monitors the heart’s rhythm and delivers an electrical shock to restore normal heart rhythm if an abnormal heartbeat is detected.
Here is a general overview of the steps involved in the ICD implantation procedure:
- Preparation: Before the procedure, the patient is given anesthesia to help them relax and reduce any pain or discomfort. The patient’s vital signs are monitored, and any necessary medical equipment is attached, such as an ECG machine.
- Accessing the heart: The ICD is inserted through a small incision in the chest and guided through the blood vessels into the heart. X-ray or ultrasound imaging is used to guide the ICD to the appropriate location within the heart.
- Placement of the leads: Once the ICD is positioned in the heart, one or more leads or wires are threaded through a vein into the heart and positioned in the appropriate location. The leads are then connected to the ICD.
- Testing and programming: The ICD is tested to ensure that it is functioning correctly and programmed to detect and treat arrhythmias appropriately. This may involve inducing an abnormal heart rhythm and then using the ICD to deliver an electrical shock to restore normal heart rhythm.
- Closure: The incision is closed with sutures or staples, and a sterile dressing is applied to the incision site.
- Recovery: After the procedure, the patient will need to stay in the hospital for a short time to recover. The patient may experience some pain or discomfort at the incision site, and the patient may need to avoid certain activities, such as lifting heavy objects, for a short time after the procedure. The ICD will be monitored and programmed regularly in follow-up appointments to ensure it continues to function correctly and provide effective treatment for arrhythmias.
Overall, the ICD implantation procedure is a minimally invasive treatment that can be highly effective in treating life-threatening arrhythmias. The procedure can take a few hours, and the patient can usually return home on the same day or the next day after the procedure.
ATHEROSCLEROSIS
Atherosclerosis is a condition in which plaque builds up inside the arteries, narrowing and hardening them. Plaque is a mixture of cholesterol, fat, calcium, and other substances that can accumulate in the artery walls. Over time, this buildup can narrow and harden the arteries, reducing blood flow and oxygen supply to the body’s organs and tissues.
The exact cause of atherosclerosis is not fully understood, but it is believed to be related to a combination of genetic, lifestyle, and environmental factors. Risk factors for atherosclerosis include:
- High blood pressure
- High cholesterol levels
- Diabetes
- Smoking
- Obesity
- Sedentary lifestyle
- Family history of heart disease
Atherosclerosis can develop slowly over time, and it may not cause any symptoms until the condition has progressed significantly. Common symptoms of atherosclerosis may include chest pain or discomfort, shortness of breath, fatigue, weakness, dizziness, and difficulty with physical activity.
Complications of atherosclerosis can include heart attack, stroke, peripheral artery disease, and aneurysm. Treatment for atherosclerosis may include lifestyle changes such as a healthy diet and regular exercise, medication to control risk factors such as high blood pressure and cholesterol, and in some cases, surgery or other invasive procedures to open or bypass blocked arteries.
Prevention of atherosclerosis is important, and it can be achieved through healthy lifestyle choices such as maintaining a healthy weight, eating a balanced and nutritious diet, getting regular exercise, not smoking, and managing underlying medical conditions such as high blood pressure and diabetes.
Treatments
The treatment for atherosclerosis aims to reduce the risk of complications such as heart attack and stroke, relieve symptoms, and improve overall cardiovascular health. Here are some common treatments for atherosclerosis:
- Lifestyle changes: Lifestyle changes are the first-line treatment for atherosclerosis. This includes adopting a heart-healthy diet that is low in saturated and trans fats, high in fiber and fruits and vegetables, getting regular exercise, quitting smoking, and managing underlying medical conditions such as high blood pressure, high cholesterol, and diabetes.
- Medications: Medications are used to treat underlying risk factors such as high blood pressure, high cholesterol, and diabetes. Medications may include statins, aspirin, beta-blockers, ACE inhibitors, and calcium channel blockers.
- Angioplasty and stenting: Angioplasty is a procedure in which a catheter with a small balloon is inserted into the blocked artery and inflated to widen the artery and restore blood flow. A stent may also be inserted to help keep the artery open.
- Coronary artery bypass surgery: This procedure involves bypassing the blocked portion of the artery by grafting a healthy vein or artery around the blockage.
- Lifestyle interventions: Several lifestyle interventions, such as consuming omega-3 fatty acids, supplements, and antioxidants, have been suggested to help reduce the risk of atherosclerosis.
It is essential to talk to a healthcare provider to determine the best treatment plan for atherosclerosis as it varies based on the severity of the condition, age, overall health, and other factors.
Tests and Procedures to diagnose Atherosclerosis
Atherosclerosis can be diagnosed through various tests and procedures, including:
- Physical exam: During a physical exam, a healthcare provider may check for signs of atherosclerosis, such as a weak pulse, a bruit (abnormal sound) heard with a stethoscope over the artery, and signs of peripheral artery disease.
- Blood tests: Blood tests can measure cholesterol levels, triglycerides, and blood sugar levels, which are all risk factors for atherosclerosis.
- Electrocardiogram (ECG or EKG): This test measures the electrical activity of the heart and can detect any abnormalities in heart rhythm.
- Echocardiogram: This test uses sound waves to create images of the heart, which can help identify any problems with the heart’s structure or function that may be related to atherosclerosis.
- Stress test: A stress test is performed to measure the heart’s response to physical activity. The test involves exercising on a treadmill or stationary bike while the heart rate and blood pressure are monitored.
- CT scan or MRI: These imaging tests can help identify any blockages or narrowing of the arteries.
- Angiography: This test involves injecting a contrast dye into the arteries and taking X-ray images to visualize the blood flow in the arteries.
- Ankle-brachial index (ABI) test: This test measures the blood pressure in the arms and legs to check for peripheral artery disease, which is often caused by atherosclerosis.
Diagnosing atherosclerosis early is crucial for effective treatment and prevention of complications. It is important to talk to a healthcare provider about any symptoms or risk factors for atherosclerosis to determine if any testing is necessary.
Medications
Medications can be used to treat atherosclerosis by managing underlying risk factors and preventing complications. Here are some common medications used for atherosclerosis:
- Statins: Statins are a class of drugs that lower cholesterol levels in the blood. They work by blocking the enzyme responsible for producing cholesterol in the liver. Statins can help reduce the risk of heart attack and stroke in people with atherosclerosis.
- Antiplatelet agents: Antiplatelet agents such as aspirin and clopidogrel are used to prevent blood clots from forming in the arteries. They work by reducing the stickiness of platelets, which are cells that can clump together and form clots in the arteries.
- Blood pressure medications: Blood pressure medications such as ACE inhibitors, beta-blockers, and calcium channel blockers can be used to manage high blood pressure, which is a major risk factor for atherosclerosis.
- Diabetes medications: Diabetes medications such as metformin, insulin, and GLP-1 receptor agonists can be used to manage blood sugar levels in people with diabetes, which is also a risk factor for atherosclerosis.
- Niacin: Niacin is a B vitamin that can help raise HDL cholesterol (the “good” cholesterol) levels in the blood. It can also lower triglycerides and LDL cholesterol levels.
- Fibrates: Fibrates are medications that can help lower triglyceride levels and raise HDL cholesterol levels.
- Ezetimibe: Ezetimibe is a medication that can help lower LDL cholesterol levels by blocking the absorption of cholesterol in the small intestine.
It is essential to talk to a healthcare provider before taking any medications for atherosclerosis to determine the most appropriate treatment plan based on individual health and medical history.
Procedure for Coronary artery bypass surgery
Coronary artery bypass surgery (CABG) is a procedure used to treat atherosclerosis by rerouting blood flow around the blocked or narrowed arteries. Here is an overview of the procedure:
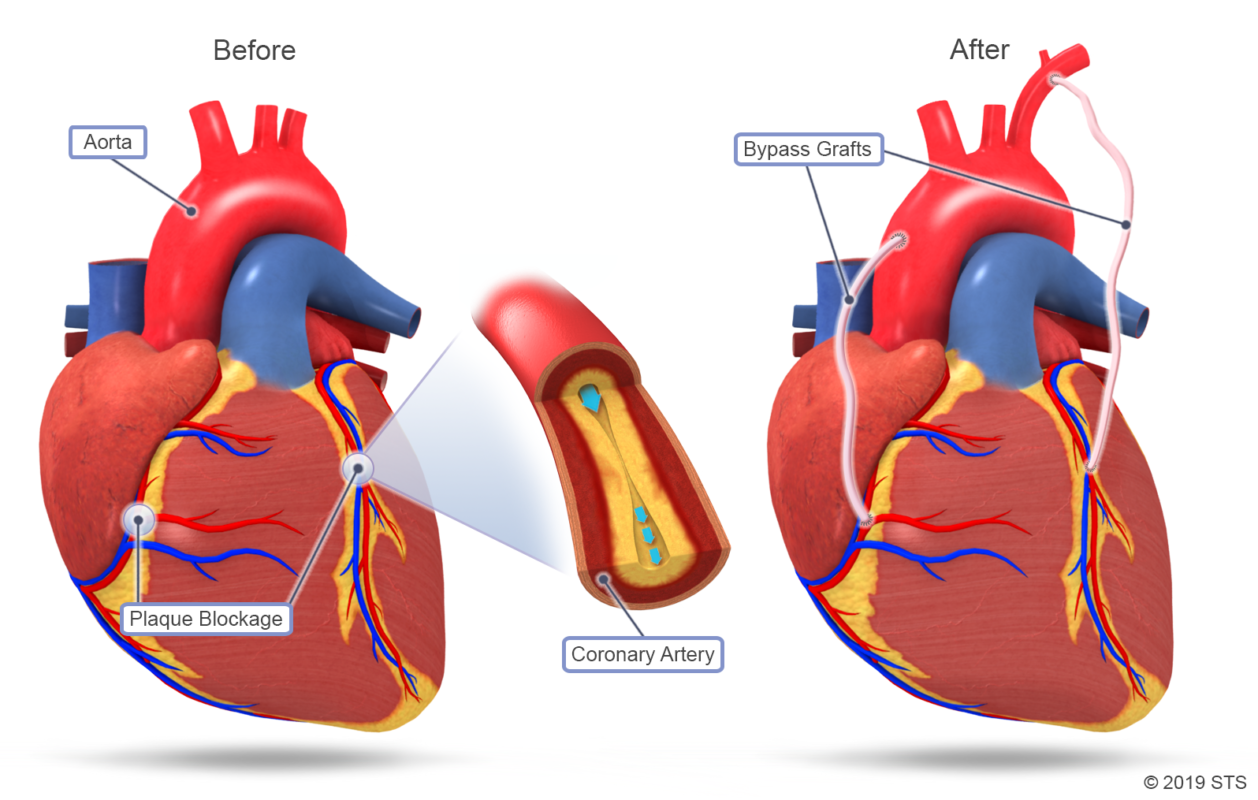
- Anesthesia: The patient is given general anesthesia to put them to sleep and prevent pain during the procedure.
- Incision: The surgeon makes an incision in the chest, usually in the middle of the chest, to access the heart.
- Harvesting of the graft: A healthy blood vessel, usually from the leg or chest, is harvested to use as a bypass graft. The vessel is carefully removed and prepared for use.
- Placement of the bypass graft: The surgeon then creates a new pathway for blood to flow around the blocked or narrowed artery by grafting the harvested vessel onto the coronary artery.
- Completion: Once all necessary bypass grafts have been placed, the surgeon checks for bleeding and closes the chest incision with sutures or staples.
After the procedure, the patient is taken to a recovery room where they will be closely monitored for any complications. The patient will likely stay in the hospital for several days to recover and may require rehabilitation to regain strength and mobility. Medications to manage pain, prevent infection, and reduce the risk of blood clots may be prescribed. Follow-up appointments will be scheduled to monitor recovery and assess ongoing symptoms.
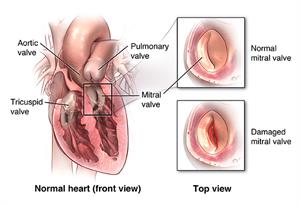
HEART VALVE DISEASE
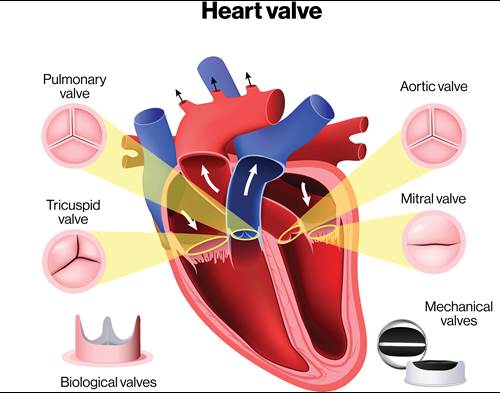
Heart valve disease is a condition in which one or more of the valves in the heart do not function properly. The heart has four valves: the mitral valve, the tricuspid valve, the pulmonary valve, and the aortic valve. These valves control the flow of blood through the heart, and when they are not working correctly, it can lead to a range of symptoms and complications.
There are two types of heart valve disease: stenosis and regurgitation. Stenosis occurs when the valve opening narrows, making it difficult for blood to flow through. Regurgitation occurs when the valve does not close properly, allowing blood to flow backward instead of forward.
Heart valve disease can be caused by a variety of factors, including congenital defects, infections, aging, and certain medical conditions. Symptoms can include shortness of breath, chest pain, fatigue, dizziness, and swelling in the ankles or feet.
Diagnosis of heart valve disease typically involves a physical exam, imaging tests such as echocardiography, and possibly a cardiac catheterization or other specialized tests. Treatment options may include medications to manage symptoms, surgery to repair or replace the valve, or minimally invasive procedures such as balloon valvuloplasty or transcatheter aortic valve replacement (TAVR). It is essential to work with a healthcare provider to determine the most appropriate treatment plan based on individual health and medical history.
Treatments
The treatment for heart valve disease depends on the severity and type of the condition, as well as the patient’s overall health and medical history. Here are some common treatments:
- Medications: Medications can help manage symptoms of heart valve disease, such as high blood pressure or heart failure. They can also help prevent blood clots or reduce the risk of infections.
- Valve repair or replacement surgery: In some cases, the damaged heart valve can be repaired surgically. In other cases, the valve may need to be replaced with a prosthetic valve, either mechanical or biological. Surgery can be open-heart or minimally invasive, depending on the severity and location of the valve disease.
- Balloon valvuloplasty: This procedure involves inserting a balloon-tipped catheter into the valve and inflating it to widen the valve opening. This can help improve blood flow through the valve.
- Transcatheter aortic valve replacement (TAVR): This minimally invasive procedure involves inserting a new valve into the diseased aortic valve using a catheter inserted through an artery in the groin or chest. It can be used for some patients who are not good candidates for open-heart surgery.
- Watchful waiting: In some cases, the heart valve disease may be mild, and the patient may not have any significant symptoms. In these cases, the doctor may recommend regular monitoring to watch for any changes in the condition.
It’s important to work with a healthcare provider to determine the most appropriate treatment plan based on individual health and medical history.
Tests and Procedures to diagnose heart valve disease
- Heart valve disease is typically diagnosed through a combination of a physical exam, medical history, and various diagnostic tests. Here are some common tests and procedures used to diagnose heart valve disease:
- Echocardiogram: This is a non-invasive test that uses sound waves to create a picture of the heart’s valves and chambers. It can show how well the valves are working and detect any abnormalities.
- Electrocardiogram (ECG): This is a non-invasive test that measures the electrical activity of the heart. It can help detect irregular heart rhythms or other abnormalities.
- Chest X-ray: This can help detect any changes in the size or shape of the heart, which may be an indication of heart valve disease.
- Cardiac catheterization: This is an invasive test that involves inserting a thin, flexible tube (catheter) into a blood vessel in the groin or arm and threading it to the heart. It can help detect blockages in the coronary arteries or abnormalities in the heart valves.
- MRI or CT scan: These imaging tests can provide detailed images of the heart and can help detect any abnormalities in the heart valves.
- Exercise stress test: This test involves exercising on a treadmill or stationary bike while being monitored to see how the heart responds to physical activity.
- Transesophageal echocardiogram (TEE): This is an invasive test that involves inserting a probe down the throat to get a closer look at the heart valves.
It’s important to work with a healthcare provider to determine which tests and procedures are necessary based on individual health and medical history.
Medications
Medications may be prescribed to help manage symptoms of heart valve disease or to reduce the risk of complications. The type of medication prescribed will depend on the type and severity of the valve disease, as well as the individual’s overall health and medical history. Here are some common medications used for heart valve disease:
- Diuretics: These medications help the body get rid of excess fluid and can be used to treat swelling or shortness of breath.
- ACE inhibitors or angiotensin receptor blockers (ARBs): These medications can help lower blood pressure and may be used to treat valve disease associated with high blood pressure.
- Beta-blockers: These medications can help slow the heart rate and reduce the workload on the heart, which can be beneficial for certain types of heart valve disease.
- Anticoagulants: These medications can help prevent blood clots and are often prescribed for patients with heart valve disease who are at risk for stroke or other complications.
- Antibiotics: These medications may be prescribed to prevent bacterial infections, which can be a risk for some patients with heart valve disease who undergo certain medical procedures.
- Statins: These medications can help lower cholesterol levels and may be prescribed for patients with heart valve disease who are at risk for cardiovascular disease.
It’s important to follow the healthcare provider’s instructions and take medications as prescribed. In some cases, medication may be used in combination with other treatments, such as surgery or minimally invasive procedures, to manage heart valve disease.
Procedure for Valve repair or replacement surgery
Valve repair or replacement surgery is a procedure performed to treat heart valve disease. The type of surgery performed will depend on the type and severity of the valve disease, as well as the individual’s overall health and medical history. Here are the general steps involved in valve repair or replacement surgery:
- Anesthesia: The patient is given general anesthesia, which means they are asleep and pain-free during the surgery.
- Incision: A surgical incision is made in the chest to access the heart. The incision may be made in the middle of the chest (sternotomy) or on the side of the chest (thoracotomy).
- Cardiopulmonary bypass: The surgeon will connect the patient to a heart-lung machine, which will temporarily take over the function of the heart and lungs. This allows the surgeon to stop the heart and perform the necessary repairs or replacements.
- Valve repair: If possible, the surgeon will attempt to repair the damaged valve by reshaping, repairing, or reinforcing the valve leaflets. This may involve using sutures or patches to repair the valve.
- Valve replacement: If the valve cannot be repaired, it will need to be replaced. The surgeon will remove the damaged valve and replace it with a prosthetic valve, either mechanical or biological.
- Closing the incision: Once the repairs or replacements are complete, the surgeon will close the incision with sutures or staples.
- Recovery: The patient will be monitored closely in the intensive care unit (ICU) for a period of time after the surgery. They may need to stay in the hospital for several days or longer, depending on the type of surgery and how well they are recovering.
It’s important to follow the healthcare provider’s instructions for postoperative care and attend follow-up appointments as scheduled. Rehabilitation may be necessary to regain strength and endurance after the surgery.
Procedure for Balloon valvuloplasty
Balloon valvuloplasty is a minimally invasive procedure performed to treat stenosis (narrowing) of a heart valve, most commonly the mitral or pulmonary valve. The procedure involves the following steps:
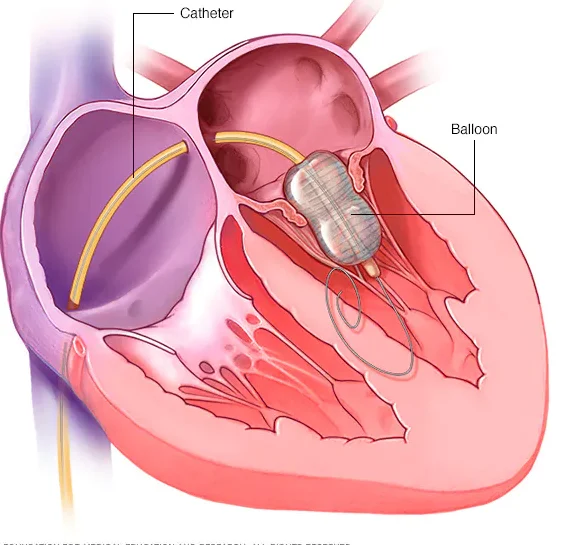
- Anesthesia: The patient is given local anesthesia and mild sedation to keep them comfortable during the procedure.
- Insertion of a catheter: A thin, flexible tube (catheter) is inserted into a blood vessel, usually in the groin area, and guided through the blood vessels to the heart valve.
- Inflation of a balloon: A deflated balloon attached to the catheter is positioned across the narrow valve opening. The balloon is then inflated to push the valve leaflets apart and widen the opening.
- Monitoring: The healthcare provider monitors the patient’s blood pressure, heart rate, and oxygen levels throughout the procedure to ensure their safety.
- Deflation and removal of the balloon: After the valve has been widened, the balloon is deflated and removed, and the catheter is withdrawn.
- Recovery: The patient is monitored for a period of time after the procedure and may need to stay in the hospital for a short time for observation.
Balloon valvuloplasty can provide relief from symptoms and improve blood flow through the affected valve. However, the effects of the procedure may not be permanent and the valve may eventually narrow again. In some cases, valve replacement surgery may be necessary.
Procedure for Transcatheter aortic valve replacement (TAVR)
Transcatheter aortic valve replacement (TAVR) is a minimally invasive procedure used to replace a damaged aortic valve in the heart without open-heart surgery. Here are the general steps involved in TAVR:
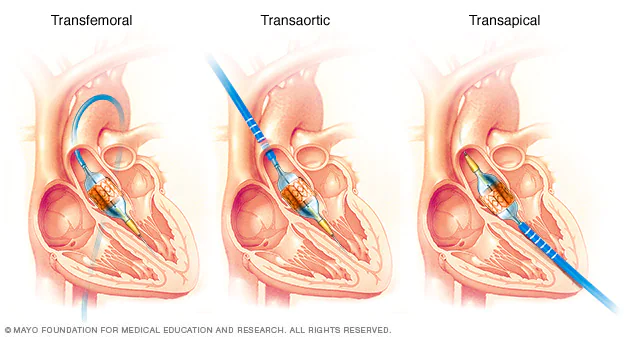
- Anesthesia: The patient is given general anesthesia, which means they are asleep and pain-free during the procedure.
- Insertion of a catheter: A thin, flexible tube (catheter) is inserted into a blood vessel, usually in the groin area, and guided through the blood vessels to the aortic valve.
- Placement of the replacement valve: Once the catheter is in place, the new valve is inserted into the catheter and guided to the site of the diseased valve. The new valve is then expanded to push the old valve aside and take over its function.
- Monitoring: The healthcare provider monitors the patient’s blood pressure, heart rate, and oxygen levels throughout the procedure to ensure their safety.
- Removal of the catheter: Once the new valve is in place, the catheter is removed and the insertion site is closed with sutures or a closure device.
- Recovery: The patient is monitored closely in the intensive care unit (ICU) for a period of time after the procedure. They may need to stay in the hospital for several days or longer, depending on how well they are recovering.
TAVR is a newer and less invasive alternative to traditional open-heart surgery for the treatment of aortic valve disease. It is typically used for patients who are considered high-risk or inoperable for traditional surgery. However, not all patients are suitable candidates for TAVR, and the healthcare provider will determine the best treatment option based on the individual’s specific situation.
CARDIOMYOPATHY
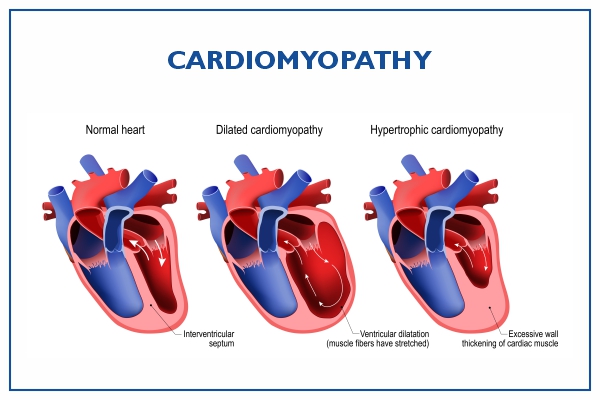
Cardiomyopathy is a term used to describe diseases of the heart muscle, which can lead to heart failure or other complications.
Cardiomyopathy can have various causes, including genetic factors, infections, drug and alcohol abuse, and other medical conditions such as hypertension and diabetes. Symptoms can include shortness of breath, chest pain, fatigue, dizziness, and swelling in the legs and feet.
Treatment for cardiomyopathy depends on the type and severity of the condition. Medications such as beta blockers, ACE inhibitors, and diuretics may be used to manage symptoms and improve heart function. In more severe cases, surgery, implantable devices such as pacemakers or defibrillators, or heart transplantation may be necessary. Lifestyle changes such as quitting smoking, reducing alcohol intake, and exercising regularly can also help manage symptoms and improve overall health.
Treatments
Treatment for cardiomyopathy depends on the type and severity of the condition. Some possible treatments for cardiomyopathy include:
- Medications: Several medications may be used to manage symptoms and improve heart function. These include beta blockers, ACE inhibitors, angiotensin receptor blockers (ARBs), aldosterone antagonists, and diuretics. In some cases, antiarrhythmic drugs may be used to control abnormal heart rhythms.
- Implantable devices: In some cases, implantable devices such as pacemakers, implantable cardioverter-defibrillators (ICDs), or biventricular pacemakers may be used to help the heart function properly.
- Surgery: In some cases, surgery may be necessary to treat cardiomyopathy. This may include procedures such as septal myectomy or alcohol septal ablation for hypertrophic cardiomyopathy, or left ventricular assist device (LVAD) or heart transplant for severe heart failure.
- Lifestyle changes: Lifestyle changes such as quitting smoking, reducing alcohol intake, and exercising regularly can also help manage symptoms and improve overall health.
- Management of underlying conditions: If an underlying condition such as high blood pressure or diabetes is contributing to the cardiomyopathy, it is important to manage that condition as well.
It is important to work closely with a healthcare provider to determine the best treatment plan for individual cases of cardiomyopathy.
Tests and Procedures to diagnose Cardiomyopathy
There are several tests and procedures that can be used to diagnose cardiomyopathy. These may include:
- Physical exam: A healthcare provider may perform a physical exam to look for signs of heart problems, such as swelling in the legs or feet, an irregular heartbeat, or an enlarged heart.
- Electrocardiogram (ECG): An ECG is a test that measures the electrical activity of the heart. It can help detect abnormal heart rhythms and other problems.
- Echocardiogram: An echocardiogram is a type of ultrasound that uses sound waves to create images of the heart. It can help detect problems with the heart muscle, such as thickening or enlargement.
- Cardiac MRI: A cardiac MRI is a type of imaging test that uses a magnetic field and radio waves to create detailed images of the heart. It can help detect problems with the heart muscle or blood flow.
- Cardiac catheterization: A cardiac catheterization is a procedure in which a thin, flexible tube is inserted into a blood vessel in the arm, groin, or neck and guided to the heart. This test can help measure blood flow and pressure in the heart, as well as identify blockages in the arteries.
- Blood tests: Blood tests may be used to check for markers of heart damage, as well as to rule out other conditions that can cause similar symptoms.
It is important to work closely with a healthcare provider to determine the best tests and procedures for diagnosing cardiomyopathy in individual cases.
Medications
There are several medications that may be used to treat cardiomyopathy, depending on the type and severity of the condition. These medications include:
- Beta blockers: Beta blockers can help reduce the workload on the heart by slowing the heart rate and reducing blood pressure. They may also help improve heart function and reduce symptoms such as shortness of breath and chest pain.
- ACE inhibitors and ARBs: These medications help relax blood vessels and reduce blood pressure, which can help improve blood flow and reduce the workload on the heart. They may also help reduce symptoms and improve heart function.
- Aldosterone antagonists: These medications can help reduce fluid buildup in the body and improve heart function. They are often used in combination with other medications such as ACE inhibitors or ARBs.
- Diuretics: Diuretics can help reduce fluid buildup in the body and reduce symptoms such as swelling in the legs and feet.
- Antiarrhythmic drugs: Antiarrhythmic drugs may be used to control abnormal heart rhythms that can occur with certain types of cardiomyopathy.
It is important to work closely with a healthcare provider to determine the best medications for individual cases of cardiomyopathy. Some medications may have side effects or interactions with other medications, so it is important to take them as prescribed and to notify a healthcare provider of any changes in symptoms or side effects.
Procedure for Implantable Devices
The procedure for implantable devices can vary depending on the specific type of device being implanted and the individual patient’s needs. However, there are some general steps that are commonly followed in the implantation process:
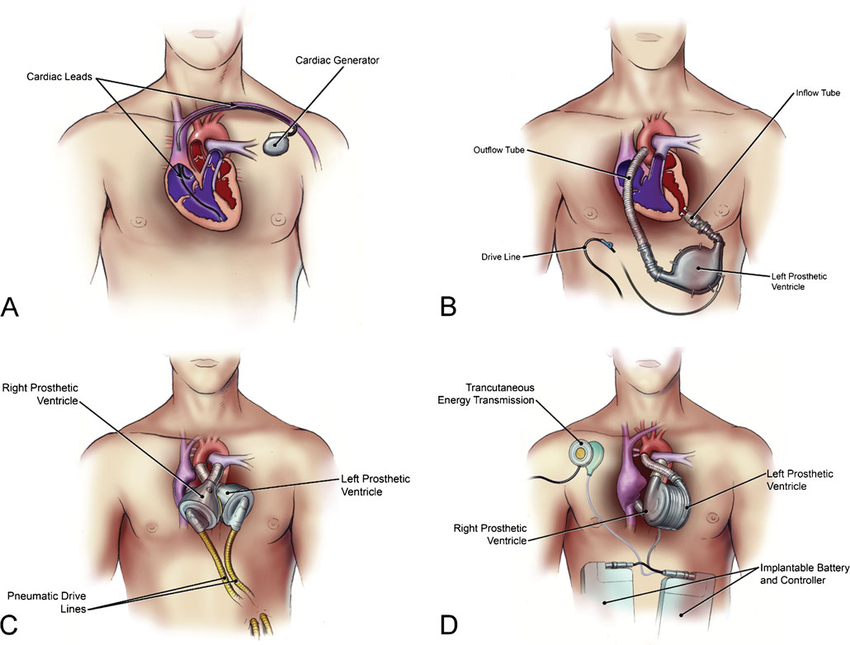
- Pre-operative evaluation: The patient will undergo a thorough evaluation to determine if they are a good candidate for the implant. This may include physical exams, imaging tests, and other diagnostic procedures.
- Anesthesia: The patient will be given anesthesia to ensure they are comfortable and pain-free during the procedure.
- Incision: The surgeon will make an incision in the skin over the area where the implant will be placed.
- Placement of the device: The surgeon will carefully place the device in the appropriate location in the body. This may involve threading wires or leads through blood vessels or other tissues.
- Testing: Once the device is in place, the surgeon will test its function to ensure it is working properly.
- Closing the incision: The surgeon will then close the incision with sutures or other closure techniques.
- Post-operative care: The patient will be closely monitored after the procedure to ensure there are no complications. This may involve pain management, antibiotics to prevent infection, and other measures as needed.
- Follow-up: The patient will need to attend follow-up appointments to monitor the function of the device and ensure there are no issues. This may involve periodic testing or other evaluations.
It’s important to note that the specific details of the procedure can vary depending on the type of implantable device being used and the patient’s individual needs. Additionally, any surgical procedure carries some risk, and patients should discuss the potential benefits and risks of implantable devices with their healthcare provider before making a decision.
Procedure for Surgery
The procedure for surgery can vary depending on the type of surgery being performed and the individual patient’s needs. However, there are some general steps that are commonly followed in most surgical procedures:
- Pre-operative evaluation: The patient will undergo a thorough evaluation to determine if they are healthy enough to undergo surgery. This may include physical exams, imaging tests, blood tests, and other diagnostic procedures.
- Anesthesia: The patient will be given anesthesia to ensure they are comfortable and pain-free during the surgery. The type of anesthesia used will depend on the type of surgery being performed and the patient’s medical history.
- Incision: The surgeon will make an incision in the skin over the area where the surgery will be performed.
- Surgery: The surgeon will carefully perform the necessary procedure, which may involve cutting, suturing, removing tissue, or other techniques depending on the type of surgery.
- Monitoring: The patient’s vital signs, such as heart rate and blood pressure, will be closely monitored throughout the surgery.
- Closing the incision: The surgeon will then close the incision with sutures or other closure techniques.
- Post-operative care: The patient will be closely monitored after the surgery to ensure there are no complications. This may involve pain management, antibiotics to prevent infection, and other measures as needed.
- Recovery: The patient will need to follow a recovery plan to help ensure proper healing. This may involve rest, physical therapy, and other measures as determined by the healthcare team.
It’s important to note that the specific details of the surgery can vary depending on the type of surgery being performed and the patient’s individual needs. Additionally, any surgical procedure carries some risk, and patients should discuss the potential benefits and risks of surgery with their healthcare provider before making a decision.
CONGENITAL HEART DISEASE

Congenital heart disease (CHD) refers to a range of structural abnormalities of the heart that are present at birth. CHD is the most common birth defect, affecting approximately 1% of live births worldwide.
The causes of CHD are not always clear, but genetic and environmental factors can play a role. Some forms of CHD may be caused by a genetic mutation or abnormality, while others may result from exposure to certain medications or environmental toxins during fetal development.
Symptoms of CHD can vary depending on the type and severity of the condition, but may include difficulty breathing, fatigue, poor growth, and blue-tinted skin (cyanosis). Treatment for CHD may include medication, surgery, or other procedures to repair or replace damaged or abnormal structures in the heart.
With proper treatment and management, many people with CHD can lead healthy and fulfilling lives. However, CHD is a lifelong condition that requires ongoing monitoring and care by a healthcare provider.
Treatments
The treatment for congenital heart disease (CHD) depends on the specific type and severity of the condition. In some cases, no treatment may be required, while in others, surgical or medical intervention may be necessary.
Here are some of the common treatments for CHD:
- Medications: Some medications may be prescribed to manage the symptoms of CHD. For example, diuretics may be used to reduce fluid build-up in the lungs, and medications that relax blood vessels may be used to reduce strain on the heart.
- Catheter-based procedures: In some cases, minimally invasive catheter-based procedures may be used to repair or replace abnormal structures in the heart. For example, a device may be inserted into the heart to close a hole, or a balloon may be inflated to widen a narrowed blood vessel.
- Surgery: Surgery may be necessary to repair or replace abnormal structures in the heart. For example, surgeons may repair a hole in the heart or replace a defective valve.
- Heart transplant: In rare cases, a heart transplant may be necessary if the CHD is severe and other treatments are not effective.
- In addition to these treatments, people with CHD may need ongoing monitoring and management by a healthcare provider. This may involve regular checkups, imaging tests, and other procedures to assess the function of the heart and monitor for complications.
It’s important to note that the specific treatment for CHD will vary depending on the individual case. People with CHD should work closely with their healthcare provider to determine the most appropriate treatment plan for their needs.
Tests and Procedures to diagnose congenital heart disease
There are several tests and procedures that can be used to diagnose congenital heart disease (CHD), including:
- Echocardiogram: This is a type of ultrasound that uses sound waves to create images of the heart. An echocardiogram can show the size and shape of the heart and can help identify any structural abnormalities.
- Electrocardiogram (ECG): This is a test that records the electrical activity of the heart. An ECG can show abnormal rhythms, which may indicate CHD.
- Chest X-ray: A chest X-ray can provide an image of the heart and lungs, which can help identify any abnormalities or fluid buildup.
- Cardiac catheterization: This is an invasive procedure that involves inserting a thin tube (catheter) into a blood vessel and threading it up to the heart. This procedure can help identify the location and severity of any structural abnormalities in the heart.
- MRI or CT scan: These imaging tests can provide detailed images of the heart and can help identify any structural abnormalities.
- Pulse oximetry: This is a non-invasive test that measures the oxygen saturation in the blood. Low oxygen levels may indicate CHD.
- Genetic testing: In some cases, genetic testing may be done to look for genetic abnormalities that may cause CHD.
It’s important to note that the specific tests and procedures used to diagnose CHD will depend on the individual case. A healthcare provider may use one or more of these tests to help diagnose CHD and develop an appropriate treatment plan. Early detection and treatment of CHD can help improve outcomes and reduce the risk of complications.
Medications
The medications used to treat congenital heart disease (CHD) will depend on the specific type and severity of the condition, as well as the individual’s overall health status. Here are some common medications used to manage CHD:
- Diuretics: These medications help reduce fluid buildup in the lungs and other parts of the body, which can be a symptom of some types of CHD.
- ACE inhibitors and beta blockers: These medications can help improve the function of the heart and reduce strain on the heart.
- Anticoagulants: These medications help prevent blood clots, which can be a risk for people with certain types of CHD.
- Digoxin: This medication helps strengthen the heartbeat and can be used to treat certain types of CHD.
- Prostaglandin E1: This medication may be used in new born with certain types of CHD to keep a blood vessel open and improve blood flow.
It’s important to note that the specific medications used to treat CHD will depend on the individual case. A healthcare provider will determine the most appropriate medication based on the type and severity of the CHD and the individual’s overall health status. People with CHD should work closely with their healthcare provider to manage their condition and follow all medication instructions carefully.
Procedure for Catheter-based procedures
Catheter-based procedures, also known as interventional procedures, are minimally invasive procedures that use catheters (thin, flexible tubes) to access the heart and blood vessels. These procedures can be used to diagnose and treat various types of heart conditions, including congenital heart disease (CHD). Here is a general overview of the catheter-based procedure process:
- Preparation: Before the procedure, the individual will receive instructions from their healthcare provider about how to prepare. This may include fasting before the procedure and temporarily stopping certain medications.
- Anesthesia: Most catheter-based procedures are performed under local anesthesia, which numbs the area around the catheter insertion site. Some procedures may require general anesthesia, which puts the individual to sleep.
- Catheter insertion: The catheter is inserted into a blood vessel, typically in the groin or arm, and guided up to the heart. The catheter may contain a balloon or other device for the procedure.
- Imaging: Imaging tests, such as X-rays or echocardiograms, are used to guide the catheter to the correct location in the heart.
- Procedure: Once the catheter is in the correct location, the procedure can begin. For example, a balloon may be inflated to widen a narrowed blood vessel, or a device may be inserted to close a hole in the heart.
- Recovery: After the procedure, the catheter is removed and the insertion site is bandaged. The individual will typically need to lie still for a few hours to prevent bleeding.
- Follow-up: The individual will be monitored for a period of time after the procedure to ensure there are no complications. They may also need additional imaging tests or check-ups to monitor the effectiveness of the procedure.
It’s important to note that the specific catheter-based procedure used to treat CHD will depend on the individual case. A healthcare provider will determine the most appropriate procedure based on the type and severity of the CHD and the individual’s overall health status. People undergoing catheter-based procedures should work closely with their healthcare provider to understand the risks and benefits of the procedure and follow all instructions carefully.
Procedure for Surgery
The procedure for surgery varies depending on the type of surgery being performed, but here is a general overview of the steps involved:
- Preoperative preparation: Before surgery, the individual will typically meet with their healthcare provider to discuss the procedure and receive instructions on how to prepare. This may include fasting before the procedure and temporarily stopping certain medications.
- Anesthesia: The individual will receive anesthesia to put them to sleep during the surgery. The type of anesthesia used will depend on the specific surgery and the individual’s overall health status.
- Incision: The surgeon will make an incision in the appropriate location to access the surgical site.
- Procedure: The surgeon will perform the necessary surgical steps to address the condition or injury. This may involve removing tissue, repairing damage, or replacing a damaged organ or structure.
- Closure: Once the procedure is complete, the surgeon will close the incision using sutures or staples.
- Recovery: The individual will be monitored in a recovery area as they wake up from anesthesia. Depending on the surgery, they may need to stay in the hospital for a period of time for further monitoring and recovery.
- Follow-up: After leaving the hospital, the individual will typically have follow-up appointments with their healthcare provider to monitor their recovery and ensure there are no complications.
It’s important to note that the specific procedure for surgery will depend on the type of surgery being performed and the individual’s overall health status. People undergoing surgery should work closely with their healthcare provider to understand the risks and benefits of the procedure and follow all instructions carefully.
Procedure for Heart Transplant
The procedure for a heart transplant involves several steps:
- Evaluation: Before a heart transplant can be performed, the individual will undergo a thorough evaluation to determine if they are a candidate for the procedure. This evaluation may include medical tests and imaging to assess the individual’s heart function and overall health status.
- Waiting for a donor heart: Once the individual is determined to be a candidate for a heart transplant, they will be placed on a waiting list for a donor heart. The wait time can vary widely depending on factors such as the individual’s blood type and the availability of donor hearts.
- Surgery preparation: When a donor heart becomes available, the individual will be called in for surgery. They will undergo preoperative preparation, which may include fasting and medication adjustments.
- Anesthesia: The individual will receive anesthesia to put them to sleep during the surgery.
- Incision: The surgeon will make an incision in the chest to access the heart.
- Removal of the diseased heart: The surgeon will remove the individual’s diseased heart.
- Implantation of the donor heart: The donor heart will be implanted and connected to the individual’s blood vessels and other structures.
- Closing the incision: Once the transplant is complete, the surgeon will close the incision using sutures or staples.
- Recovery: The individual will be monitored in a recovery area as they wake up from anesthesia. They will then be transferred to a hospital room for further monitoring and recovery.
- Follow-up: After leaving the hospital, the individual will have frequent follow-up appointments with their healthcare provider to monitor their recovery and ensure that their body is not rejecting the donor heart. They will also need to take immunosuppressive medications to prevent rejection of the donor heart for the rest of their life.
It’s important to note that a heart transplant is a complex and highly specialized procedure that carries significant risks. People undergoing a heart transplant should work closely with their healthcare provider to understand the risks and benefits of the procedure and follow all instructions carefully.
MYOCARDITIS
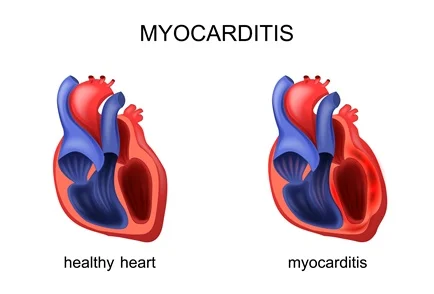
Myocarditis is a condition in which the heart muscle (myocardium) becomes inflamed, which can weaken the heart and cause a variety of symptoms. It can be caused by a viral, bacterial, or fungal infection, or as a result of an autoimmune disorder.
Symptoms of myocarditis can include:
- Fatigue
- Shortness of breath
- Chest pain or discomfort
- Rapid or irregular heartbeat
- Swelling in the legs, ankles, or feet
- Light-headedness or fainting
- Flu-like symptoms, such as fever, headache, and muscle aches
Myocarditis can range in severity from mild and self-limiting to severe and life-threatening. In some cases, it can cause permanent damage to the heart muscle, leading to heart failure.
Diagnosis of myocarditis typically involves a combination of medical history, physical exam, and medical tests, such as blood tests, electrocardiogram (ECG), echocardiogram, and cardiac magnetic resonance imaging (MRI).
Treatment of myocarditis depends on the underlying cause and severity of the condition. In some cases, supportive care, such as rest and medications to manage symptoms, may be all that is needed. In more severe cases, hospitalization and treatment with intravenous medications or mechanical support devices may be necessary.
It’s important to seek medical attention if you experience any symptoms of myocarditis, as early diagnosis and treatment can help prevent complications and improve outcomes.
Treatments
The treatment for myocarditis depends on the underlying cause and the severity of the condition. In some cases, mild myocarditis may resolve on its own without treatment. However, in more severe cases, treatment may be necessary to manage symptoms and prevent complications. Here are some common treatments for myocarditis:
- Rest: Rest is an important part of the treatment for myocarditis. Individuals with myocarditis are advised to rest and avoid strenuous activities that can put stress on the heart.
- Medications: Medications may be prescribed to manage symptoms of myocarditis, such as fever, pain, and inflammation. Examples of medications that may be used include nonsteroidal anti-inflammatory drugs (NSAIDs), corticosteroids, and immunosuppressive drugs.
- Treat the underlying infection: If the myocarditis is caused by a bacterial, viral, or fungal infection, antibiotics or antiviral medications may be prescribed to treat the underlying infection.
- Manage heart failure: In cases where myocarditis has led to heart failure, medications such as diuretics, ACE inhibitors, and beta-blockers may be used to manage symptoms and improve heart function.
- Mechanical support: In some severe cases of myocarditis, mechanical support devices such as an intra-aortic balloon pump or a left ventricular assist device may be used to help the heart pump blood.
- Heart transplant: In very rare cases where the myocarditis has caused severe damage to the heart and other treatments have been unsuccessful, a heart transplant may be considered.
It’s important to work closely with your healthcare provider to determine the most appropriate treatment plan for your specific situation. With proper treatment and management, many people with myocarditis are able to recover fully and resume their normal activities.
Tests and Procedures to diagnose Myocarditis
There are several tests and procedures that can be used to diagnose myocarditis. These include:
- Medical history and physical exam: The doctor will ask questions about your symptoms and medical history and perform a physical exam to check for signs of myocarditis, such as a rapid or irregular heartbeat, abnormal heart sounds, or fluid buildup in the lungs.
- Blood tests: Blood tests can be done to check for signs of inflammation or infection, such as elevated levels of white blood cells or certain proteins.
- Electrocardiogram (ECG): This test measures the electrical activity of the heart and can detect abnormal heart rhythms or other signs of heart damage.
- Echocardiogram: This is an imaging test that uses sound waves to create images of the heart. It can show the size and shape of the heart, as well as how well it is functioning.
- Cardiac magnetic resonance imaging (MRI): This test uses a powerful magnetic field and radio waves to create detailed images of the heart. It can provide more detailed information about the structure and function of the heart than other imaging tests.
- Endomyocardial biopsy: This is a procedure in which a small sample of heart tissue is removed and examined under a microscope to look for signs of inflammation or infection.
The specific tests and procedures used to diagnose myocarditis may vary depending on the individual case and the healthcare provider’s recommendations. Early diagnosis and treatment of myocarditis is important to prevent complications and improve outcomes, so it’s important to seek medical attention if you experience any symptoms of myocarditis.
Medications
Medications for myocarditis may be prescribed to manage symptoms and treat the underlying cause of the condition. The specific medications used will depend on the individual case and the underlying cause of the myocarditis. Here are some examples of medications that may be used:
- Nonsteroidal anti-inflammatory drugs (NSAIDs): These medications can help reduce pain and inflammation in the heart muscle. Examples include ibuprofen and aspirin.
- Corticosteroids: These medications can help reduce inflammation in the heart muscle and may be prescribed for more severe cases of myocarditis. Examples include prednisone and dexamethasone.
- Immunosuppressive drugs: These medications may be prescribed if the myocarditis is caused by an autoimmune disorder. They work by suppressing the immune system to prevent it from attacking the heart muscle. Examples include azathioprine and cyclosporine.
- Antibiotics: If the myocarditis is caused by a bacterial infection, antibiotics may be prescribed to treat the infection and prevent further damage to the heart muscle.
- Antiviral medications: If the myocarditis is caused by a viral infection, antiviral medications may be prescribed to help reduce inflammation and prevent further damage to the heart muscle.
- Heart failure medications: If the myocarditis has led to heart failure, medications such as diuretics, ACE inhibitors, and beta-blockers may be used to manage symptoms and improve heart function.
It’s important to work closely with your healthcare provider to determine the most appropriate medication regimen for your specific situation. Medications alone may not be enough to treat myocarditis, and additional treatments such as rest, lifestyle changes, and medical procedures may be necessary.
Procedure for Heart transplant
A heart transplant is a complex surgical procedure that involves replacing a diseased or damaged heart with a healthy heart from a deceased donor. Here is an overview of the typical steps involved in a heart transplant procedure:
- Evaluation: Before a heart transplant can be performed, the recipient will undergo a thorough medical evaluation to determine if they are a suitable candidate for the procedure. This may include blood tests, imaging tests, and other diagnostic tests to assess the condition of the heart and other organs.
- Waiting for a donor heart: Once a patient is approved for a heart transplant, they will be placed on a waiting list for a donor heart. The wait time can vary widely depending on a number of factors, including the patient’s blood type, age, and overall health, as well as the availability of donor hearts.
- Preparing for surgery: When a donor heart becomes available, the patient will be contacted and instructed to come to the hospital immediately. They will undergo additional testing and preparation for the surgery, which may include fasting, administering medications, and undergoing additional imaging tests.
- Surgery: The heart transplant surgery typically takes several hours and is performed under general anesthesia. The surgeon will make an incision in the chest and remove the patient’s diseased heart. The donor heart is then implanted and connected to the patient’s blood vessels and other tissues.
- Recovery: After the surgery, the patient will be closely monitored in the intensive care unit for several days. They may need to stay in the hospital for several weeks or longer to recover from the surgery and receive post-operative care.
- Follow-up care: After being discharged from the hospital, the patient will need to undergo regular follow-up appointments with their healthcare provider to monitor their progress and ensure that their new heart is functioning properly. They will also need to take medications to prevent their body from rejecting the donor heart.
It’s important to note that a heart transplant is a major surgical procedure with significant risks and potential complications. However, for patients with advanced heart disease, it can be a life-saving treatment option. The decision to undergo a heart transplant should be carefully considered in consultation with a healthcare provider.
HYPERTENSIVE HEART DISEASE
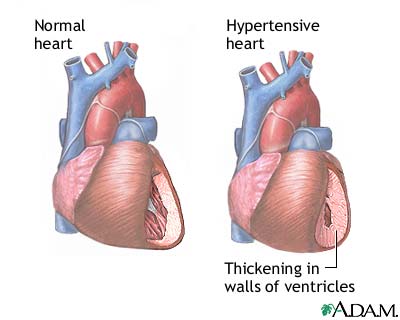
Hypertensive heart disease refers to a group of conditions that occur as a result of long-term high blood pressure (hypertension) affecting the heart. Over time, high blood pressure can cause the heart to work harder than normal, leading to damage to the heart muscle, blood vessels, and other structures in the cardiovascular system.
Some common types of hypertensive heart disease include:
- Left ventricular hypertrophy: This condition occurs when the muscle of the left ventricle (the main pumping chamber of the heart) becomes abnormally thickened as a result of high blood pressure.
- Coronary artery disease: High blood pressure can cause damage to the coronary arteries (the blood vessels that supply the heart muscle with oxygen and nutrients), leading to the development of blockages that can cause chest pain (angina), heart attack, or other serious complications.
- Heart failure: Over time, high blood pressure can cause the heart to weaken and become less efficient at pumping blood, leading to heart failure.
- Aortic aneurysm: High blood pressure can cause the aorta (the main artery that carries blood from the heart to the rest of the body) to weaken and bulge out, which can lead to a potentially life-threatening condition called an aortic aneurysm.
Treatment for hypertensive heart disease typically involves controlling high blood pressure through lifestyle changes (such as a healthy diet, regular exercise, and stress management) and medications (such as ACE inhibitors, beta blockers, and diuretics). In some cases, additional treatments such as surgery or medical procedures may be necessary to manage complications of the condition.
Treatments
The main goal of treating hypertensive heart disease is to manage high blood pressure and prevent or minimize damage to the heart and other organs. Treatment options may include:
- Lifestyle changes: Lifestyle modifications such as regular exercise, a healthy diet, weight management, and reducing salt intake can help to lower blood pressure and reduce the risk of complications associated with hypertensive heart disease.
- Medications: There are several medications available to help lower blood pressure, including diuretics, ACE inhibitors, angiotensin receptor blockers (ARBs), calcium channel blockers, and beta blockers. Your doctor may prescribe one or more of these medications based on your individual needs.
- Surgery or medical procedures: In some cases, surgery or medical procedures may be necessary to manage complications of hypertensive heart disease. For example, aortic aneurysms may require surgical repair or replacement, while coronary artery disease may be managed with angioplasty, stenting, or bypass surgery.
- Managing underlying conditions: Hypertensive heart disease is often associated with other underlying conditions such as diabetes, high cholesterol, or sleep apnea. Managing these conditions through lifestyle changes and medication may also be necessary to help lower blood pressure and reduce the risk of complications.
It’s important to work closely with your healthcare provider to develop an individualized treatment plan for hypertensive heart disease that takes into account your specific needs and medical history. Regular follow-up appointments and monitoring are also essential to ensure that treatment is effective and to adjust treatment as needed.
Tests and Procedures to diagnose Hypertensive Heart Disease
Diagnosing hypertensive heart disease typically involves a combination of a medical history, physical examination, and diagnostic tests. Some of the tests and procedures that may be used to diagnose hypertensive heart disease include:
- Blood pressure measurement: A simple blood pressure test can help to diagnose high blood pressure, which is a key factor in the development of hypertensive heart disease.
- Electrocardiogram (ECG or EKG): This test uses electrodes placed on the chest to measure the electrical activity of the heart and can help to identify any abnormal heart rhythms or patterns that may be indicative of hypertensive heart disease.
- Echocardiogram: This is an imaging test that uses sound waves to create detailed images of the heart. It can help to identify any abnormalities in the structure or function of the heart that may be related to hypertensive heart disease, such as left ventricular hypertrophy.
- Cardiac stress test: This test involves monitoring the heart while exercising or performing physical activity to help identify any abnormalities in heart function that may be associated with hypertensive heart disease.
- Cardiac catheterization: This procedure involves inserting a thin, flexible tube into a blood vessel in the arm or leg and threading it up to the heart. It can help to identify any blockages or other issues in the blood vessels of the heart that may be contributing to hypertensive heart disease.
- CT or MRI scans: These imaging tests can help to provide detailed images of the heart and surrounding blood vessels, which can be useful in identifying any structural abnormalities or damage caused by hypertensive heart disease.
It’s important to work closely with your healthcare provider to determine which diagnostic tests and procedures are appropriate for your individual needs and medical history. Early diagnosis and treatment of hypertensive heart disease can help to prevent or minimize damage to the heart and improve overall outcomes.
Medications
There are several classes of medications that may be used to treat hypertensive heart disease, including:
- Diuretics: These medications help to reduce fluid buildup in the body by increasing urine output. This can help to lower blood pressure and reduce the workload on the heart.
- ACE inhibitors: These medications work by blocking the formation of a hormone called angiotensin II, which can cause blood vessels to narrow and increase blood pressure.
- Angiotensin receptor blockers (ARBs): These medications work in a similar way to ACE inhibitors, but instead of blocking the formation of angiotensin II, they block its effects on blood vessels.
- Calcium channel blockers: These medications help to relax blood vessels and reduce the workload on the heart by blocking the movement of calcium into the heart muscle and blood vessel walls.
- Beta blockers: These medications help to slow the heart rate and reduce the force of the heart’s contractions, which can help to lower blood pressure and reduce the workload on the heart.
- Aldosterone antagonists: These medications work by blocking the effects of a hormone called aldosterone, which can cause the body to retain salt and water, increasing blood volume and blood pressure.
The specific medications that are used to treat hypertensive heart disease will depend on the individual patient’s needs and medical history. In some cases, a combination of medications may be used to achieve optimal blood pressure control and reduce the risk of complications. It’s important to work closely with your healthcare provider to develop an individualized treatment plan that is appropriate for your specific situation.
Procedure for Surgery or medical procedures
The procedure for surgery or medical procedures will depend on the specific type of procedure being performed. However, some general steps that may be involved in a surgical or medical procedure include:
- Preparation: This may involve fasting before the procedure, stopping certain medications or supplements, and undergoing any necessary tests or evaluations to assess your overall health and suitability for the procedure.
- Anesthesia: Depending on the type of procedure, you may receive local anesthesia (which numbs a specific area of the body), regional anesthesia (which numbs a larger area of the body), or general anesthesia (which puts you to sleep).
- Incision: For surgical procedures, an incision will be made in the appropriate area of the body to allow the surgeon access to the area that needs to be treated.
- Procedure: This will involve the specific steps necessary to perform the procedure, which may include removing tissue, repairing or replacing damaged structures, or inserting medical devices or instruments.
- Closing the incision: Once the procedure is complete, the incision will be closed using sutures or staples.
- Recovery: You will be monitored closely as you recover from the procedure, which may involve staying in the hospital for a period of time or undergoing outpatient care. Pain management, physical therapy, and other supportive measures may be used to help you recover as quickly and safely as possible.
It’s important to discuss the specific procedure and its associated risks, benefits, and expected outcomes with your healthcare provider, as well as any questions or concerns you may have about the procedure or its aftermath.
PERIPHERAL ARTERY DISEASE
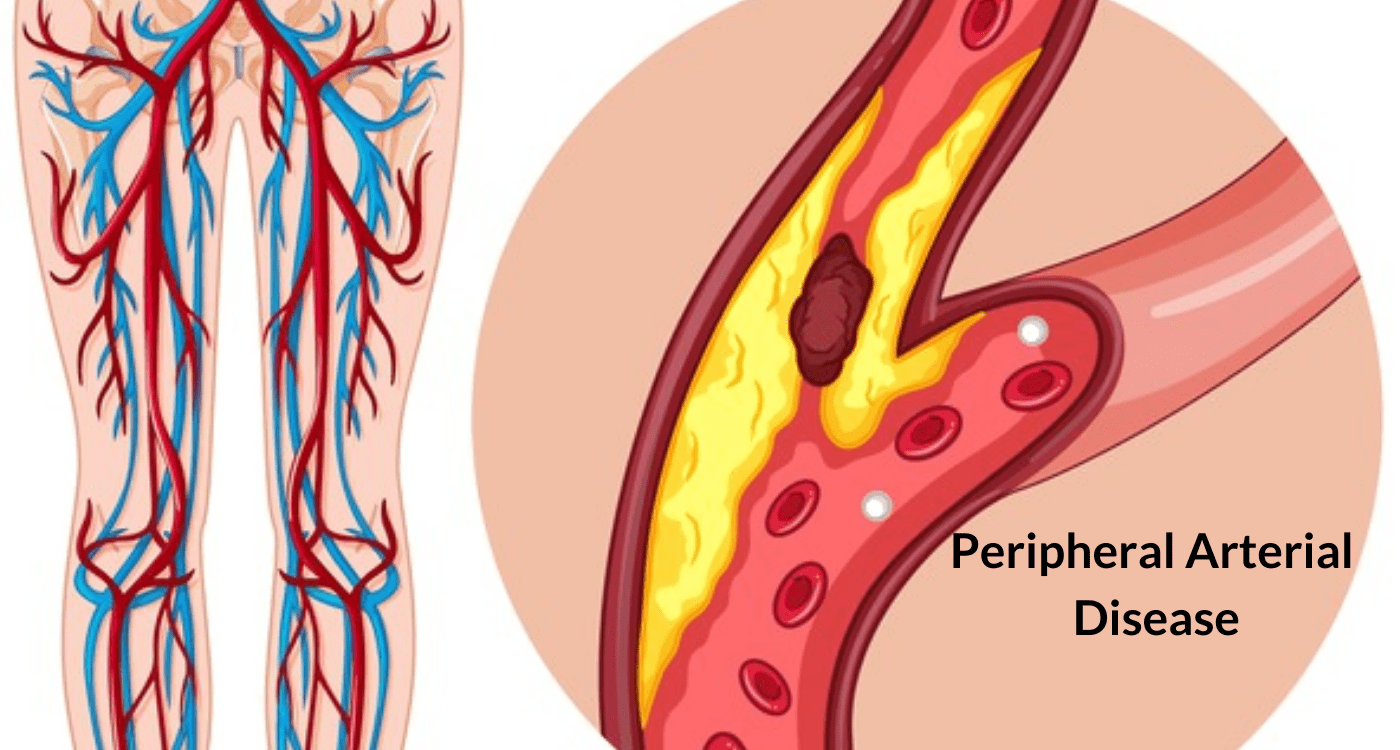
Peripheral artery disease (PAD) is a common circulatory problem that occurs when there is a build-up of plaque in the arteries that carry blood to the limbs, especially the legs. This build-up of plaque can cause the arteries to narrow or become blocked, leading to reduced blood flow to the affected areas. PAD typically affects people over the age of 50, especially those with a history of smoking, diabetes, high blood pressure, or high cholesterol.
Symptoms of PAD may include:
- Leg pain or cramping, especially during activity
- Numbness or weakness in the legs
- Coldness or pale skin in the legs
- Slow-healing sores or infections on the legs or feet
- Shiny, thin, or hairless skin on the legs
- Weak or absent pulses in the legs or feet
If left untreated, PAD can lead to serious complications, including tissue death (gangrene), infections, and even amputation. It can also increase the risk of heart attack and stroke.
Treatment for PAD may include lifestyle changes (such as quitting smoking, exercising regularly, and eating a healthy diet), medications (such as blood thinners, cholesterol-lowering drugs, and blood pressure medications), and procedures (such as angioplasty or bypass surgery) to improve blood flow to the affected areas. It’s important to work closely with your healthcare provider to develop an individualized treatment plan that is appropriate for your specific situation.
Treatments
The treatment for peripheral artery disease (PAD) depends on the severity of the condition and may include the following:
- Lifestyle changes: Quitting smoking, adopting a healthy diet, regular exercise, and weight management can help reduce symptoms of PAD and improve overall health.
- Medications: Your healthcare provider may prescribe medications to lower cholesterol, blood pressure, or blood sugar levels, as well as blood thinners to prevent blood clots from forming.
- Angioplasty: This procedure involves inflating a balloon within the narrowed artery to widen it and improve blood flow. A stent, a small metal mesh tube, may be placed within the artery to help keep it open.
- Bypass surgery: In cases where the blockage is severe, bypass surgery may be recommended. This involves taking a healthy blood vessel from another part of the body and using it to create a detour around the blocked or narrowed artery.
- Thrombolytic therapy: This treatment involves the use of medication to dissolve blood clots in the affected arteries.
- This surgical procedure involves removing plaque build-up from the inner lining of the artery.
It’s important to work closely with your healthcare provider to develop an individualized treatment plan that is appropriate for your specific situation. Maintaining a healthy lifestyle and monitoring the condition regularly can help prevent complications and improve overall health.
Tests and Procedures to diagnose Peripheral artery disease (PAD):
There are several tests and procedures that can be used to diagnose peripheral artery disease (PAD). These may include:
- Physical exam: Your healthcare provider may examine your legs and feet for signs of PAD, such as weak or absent pulses, sores, or changes in skin color or texture.
- Ankle-brachial index (ABI): This non-invasive test compares the blood pressure in your ankles to the blood pressure in your arms. A lower ankle pressure indicates a blockage in the arteries supplying blood to the legs.
- Duplex ultrasound: This non-invasive test uses high-frequency sound waves to create images of the blood vessels and measure blood flow. It can help identify areas of blockage or narrowing in the arteries.
- Magnetic resonance angiography (MRA): This imaging test uses a magnetic field and radio waves to create detailed images of the blood vessels. It can help identify blockages or narrowing in the arteries.
- Computed tomography angiography (CTA): This imaging test uses X-rays and a contrast dye to create detailed images of the blood vessels. It can help identify blockages or narrowing in the arteries.
- Angiogram: This invasive test involves injecting a contrast dye into the arteries and taking X-ray images to visualize the blood flow. It can help identify the location and severity of any blockages.
Your healthcare provider may recommend one or more of these tests based on your symptoms and medical history. Early detection and treatment of PAD can help prevent complications and improve overall health outcomes.
Medications
There are several medications that may be prescribed to manage the symptoms and slow the progression of peripheral artery disease (PAD). These may include:
- Antiplatelet drugs: These medications help prevent blood clots from forming in the arteries and reduce the risk of heart attack or stroke. Examples include aspirin, clopidogrel, and ticagrelor.
- Cholesterol-lowering drugs: These medications help lower LDL cholesterol levels and reduce the buildup of plaque in the arteries. Examples include statins, ezetimibe, and PCSK9 inhibitors.
- Blood pressure medications: These medications help lower blood pressure and reduce the workload on the heart. Examples include ACE inhibitors, ARBs, beta blockers, and calcium channel blockers.
- Blood sugar-lowering drugs: These medications help lower blood sugar levels and reduce the risk of complications associated with diabetes. Examples include metformin, sulfonylureas, and SGLT2 inhibitors.
- Cilostazol: This medication improves blood flow by preventing platelets from clumping together and dilating blood vessels.
- Pentoxifylline: This medication improves blood flow by reducing the viscosity of the blood and increasing red blood cell flexibility.
It’s important to take these medications as prescribed by your healthcare provider and to follow up regularly to monitor their effectiveness and adjust the dosage as needed. In some cases, medication alone may not be sufficient to manage the symptoms of PAD, and other treatments such as lifestyle changes or surgical procedures may be recommended.
Procedure for Bypass surgery:
Bypass surgery, also known as coronary artery bypass grafting (CABG), is a surgical procedure that is used to treat blockages in the coronary arteries. Here’s a general overview of the
Procedure
- Anesthesia: Before the surgery, the patient will be given anesthesia to make them sleep and ensure that they do not feel any pain during the procedure.
- Incision: The surgeon will make an incision in the chest, usually along the breastbone (sternum), to access the heart.
- Harvesting vein or artery: The surgeon will then harvest a vein or artery from another part of the body, such as the leg or arm. This will be used to create a bypass around the blocked or narrowed portion of the coronary artery.
- Connecting the bypass: The surgeon will then use the harvested vein or artery to create a detour around the blocked portion of the coronary artery. The bypass is connected above and below the blockage, restoring blood flow to the heart muscle.
- Closing the incision: Once the bypass is completed, the surgeon will close the incision in the chest using sutures or staples. The patient will be taken to a recovery room and monitored closely as they wake up from the anesthesia.
The procedure typically takes 3 to 6 hours to complete, and the patient will need to stay in the hospital for several days afterward to recover. Recovery time can vary depending on the patient’s overall health and the extent of the surgery. Follow-up care may include medications, lifestyle changes, and regular check-ups with a healthcare provider to monitor the patient’s heart health.
Procedure for Thrombolytic therapy
Thrombolytic therapy is a medical procedure used to dissolve blood clots that are blocking blood flow in the arteries or veins. Here’s a general overview of the procedure:
- Diagnosis: The first step in thrombolytic therapy is to diagnose the presence of a blood clot using diagnostic imaging such as ultrasound, CT scan, or angiography.
- Pre-treatment evaluation: The patient will undergo a pre-treatment evaluation to assess their overall health and determine whether thrombolytic therapy is appropriate for them. This evaluation may include a physical examination, blood tests, and an electrocardiogram (ECG).
- Administration of medication: Thrombolytic therapy involves the administration of medications known as thrombolytics, which work to dissolve the blood clot. These medications are typically given intravenously (through a vein) or, in some cases, directly into the clot through a catheter.
- Monitoring: During the procedure, the patient will be closely monitored for any signs of bleeding or other complications. They may also receive additional medications to help prevent blood clots from forming in the future.
- Post-treatment evaluation: After the procedure, the patient will undergo a post-treatment evaluation to assess the effectiveness of the thrombolytic therapy and monitor for any complications. Follow-up care may include medications, lifestyle changes, and regular check-ups with a healthcare provider to monitor the patient’s blood clotting and overall health.
It’s important to note that thrombolytic therapy carries a risk of bleeding, which can be serious or even life-threatening in some cases. As such, this procedure is typically reserved for situations where the benefits outweigh the risks, such as in cases of acute heart attack or stroke. The decision to undergo thrombolytic therapy will be made by a healthcare provider based on the individual patient’s condition and medical history.
Procedure for Endarterectomy
Endarterectomy is a surgical procedure performed to remove plaque build-up from the inner lining of an artery. The following is a general overview of the procedure:
- Anesthesia: The patient is given general anesthesia to ensure they are asleep and pain-free during the procedure.
- Incision: The surgeon makes an incision over the affected artery to gain access to the plaque buildup.
- Artery exposure: The surgeon carefully dissects the artery and exposes the plaque buildup.
- Removal of plaque: Using special surgical instruments, the surgeon removes the plaque from the inner lining of the artery. Care is taken to avoid damaging the artery or causing any fragments of plaque to break off and potentially cause further blockages.
- Closure: Once the plaque has been removed, the surgeon closes the incision using stitches or surgical staples.
- Postoperative care: After the procedure, the patient will be closely monitored for any signs of bleeding or other complications. They may also receive medications to help manage pain and prevent blood clots from forming.
Endarterectomy is commonly used to treat blockages in the carotid artery, which supplies blood to the brain. The procedure can help reduce the risk of stroke in patients with severe blockages. However, as with any surgical procedure, there are risks involved, including bleeding, infection, and damage to the artery or surrounding tissues. The decision to undergo endarterectomy will be made by a healthcare provider based on the individual patient’s condition and medical history.
ALLOPATHY CENTERS FOR ANDHRA PRADESH AND TELANGANA:
Allopathic Heart centres:
- LIVO Heart EECP Treatment Center
Address: 540, Rd Number 1, opp. GHMC Park, Kukatpally Housing Board Colony, Kukatpally, Hyderabad, Telangana 500072
- Venessha EECP Heart Care Center
Address: Kamala Prasanna Nagar, Madhavaram Nagar Colony, Kamala Prasad Nagar, Hyderabad, Telangana 500072
- Apollo Healthy Heart Doctor Hyderabad
Address: Film Nagar, Hyderabad, Telangana 500096
- Citizen’s Hospital: Cardiology Department Nallagandla
Address: F8C6+6GX, Hyderabad, Telangana 500019
- Prathima Hospitals – Best Hospital in Hyderabad
Address: 3/4/3, Kachiguda Station Rd, Barkatpura, Kachiguda, Hyderabad, Telangana 500027
- Peddeswara heart care center & multispeciality hospital
Address: 29-12-19, 29-12-21, Dornakal Road, Venkataratnam St, Moghalrajpuram, Suryaraopeta, Vijayawada, Andhra Pradesh 520002
- Heart Care Centre
Address: GJ4X+F6C, Moghalrajpuram, Christurajupuram, Vijayawada, Andhra Pradesh 520010
- Rishi Cardiac Center
Address: 9-60-102, Ganapathi Road, Kothapeta, Near Nehru Center, Vijayawada, Andhra Pradesh 520001
- SV HEART CARE CENTRE
Address: 78-10-9, Syamala Nagar, Gandhipuram, Rajamahendravaram, Andhra Pradesh 533103
Ayurvedic Heart Centres:
1. Sri Gayatri Ayurvedic Multispecialty Centre
Address: Devi Oil Mill Building, 29-7-19/1, Vishnuvardhana Rao Street, Milroad, opp. Indla Rama Subba Reddy Hospital, Suryaraopeta, Vijayawada, Andhra Pradesh 520002
2. Dr.Sumana’s SAI AYURVEDA HOSPITALS
Address: 30-22, K.P.Towers, 80, Eluru Rd, Seetharampuram, Durga Agraharam, Arundalpet, Governor Peta, Vijayawada, Andhra Pradesh 520002
- Sri Ram Mohan Ayurveda Hospital
Address: 27-37-135, MG Rd, Governor Peta, Vijayawada, Andhra Pradesh 520002
- Dhyasa Speciality Ayurvedic Clinc
Address: Dno # 23, 22-93, Sivalayam Rd, satyanarayanapuram, Vijayawada, Andhra Pradesh 520001
- Guru Dhanwantari Ayurvedic Multispeciality Center
Address: #27-10-23, atta rattiah street before sri sai mani lodge, beside road of bank of baroda, Governor Peta, Vijayawada, Andhra Pradesh 520010
- Manavaidyam Ayurveda Clinic and Panchakarma Speciality Treatment Centre
Address: 8-3-168, Bhanu Towers, Opposite ESI Hospital, beside Vijayalaxmi Temple, Erragadda, Hyderabad, Telangana 500038
- Ayurbharati Ayurveda Healthcare Centre
Address: Near Bank of Baroda ATM, Street no:8, Shivam Rd, New Nallakunta, Hyderabad, Telangana 500044
- Brundavanam Ayurvedic Clinic
Address: HIG-56, G-1, Sindhu nclave, Near Venkateshwaraswamy Temple Bus Stop, E K.P.H.B. Colony, Kukatpally ph:9848240602, eSeva Ln, Kukatpally Housing Board Colony, Kukatpally, Hyderabad, Telangana 500085
- ARADHANA AYURVEDA WELLNESS & RESEARCH CENTRE
Address: Aradhana gram, 4-3-In0001, NH 61, Nanded Road, Bhainsa, Telangana 504103
10.Radhaa’s Ayurway – Ayurveda family wellness center
Address: 3rd, Millennium Square, above ratnadeep supermarket, Lumbini Avenue, Gachibowli, Hyderabad, Telangana 500032.



